The menopausal transition is sometimes difficult to process. Many women are afraid that they will quickly deteriorate physically and mentally. In addition to the physical complaints, negative feelings sometimes arise that can affect relationships and your environment. Good information can help you get through the menopausal transition well. That's why we created this flyer, where we explain what happens in the body and the available treatment options.
Inhoud
1 General information about the menopausal transition 2
1.1 What is the period of menopausal transition? 2
1.2 What changes occur during the menopausal transition? 2
2.1 What are the consequences of the menopausal transition? 5
2.2 Which menopausal complaints may occur? 6
2.3 What other complaints are common in the years of menopausal transition? 7
2.4 Menopause and contraception 8
2.5 What are consequences of the menopausal transition - the long-term? 9
3. Menopausal symptoms and lifestyle and/or treatment 10
3.1 What can I do about menopausal symptoms? 10
3.2 What can I expect from self-care products? 12
3.3 What is a possible hormonal treatment for menopausal symptoms? 12
3.4 What are the risks of hormone treatment for women in the menopause? 15
3.5 Which non-hormonal treatment can be used? 16
1 General information about the menopausal transition
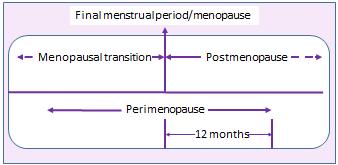
1.1 What is the period of menopausal transition?
The period of menopausal transition is the period in which menopausal symptoms such as hot flashes or (nighttime) sweating attacks can occur that are caused by reduced activity of the ovaries.
The years around the last menstrual period are called the period of menopausal transition. During this period, hormonal changes take place that are related to the changing function of the ovaries with the eventual absence of menstruation. These hormonal changes can cause all kinds of complaints. The hot flashes and night sweats are best known, but the menopausal transition can bring many more problems. The duration, type and severity of the complaints are different for every woman. One in five women is hardly bothered by these changes, but in 80% of the women, physical and/or psychological complaints develop to a greater or lesser extent during the menopause. In addition, the menopausal transition can also bring mixed feelings. Some women are relieved when the menstrual period does not come, while other women find it difficult that this means the end of the fertile stage of life.
There is no need to be hindered by menopausal symptoms; it is important to be able to be active during and after the period of menopausal transition and to have a good quality of life.
1.2 What changes occur during the menopausal transition?
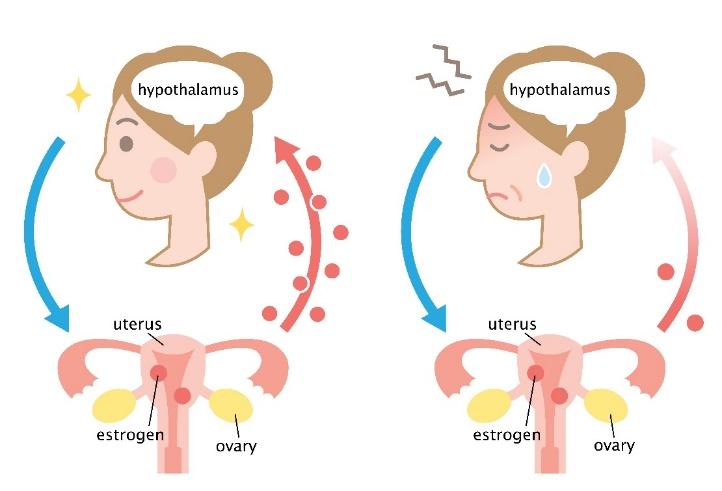
Many different types of hormones are produced in our body that are essential for communication between organs. For example, sex hormones regulate all kinds of typically female processes in the body, such as the development and functioning of sexual organs, hair growth and physique. The main female sex hormones are estrogen and progesterone. Both hormones are made by the ovaries and regulate the menstrual cycle.
Estrogens ensure that the lining of the uterus grows back every month. In addition, they affect all kinds of tissues and organs in the body, such as the heart and blood vessels, bones and skin. Progesterone ensures that the endometrium gets the right structure to receive a possibly fertilized egg. If fertilization doesn't take place, the ovaries stop making estrogen and progesterone. The endometrium is shed and drained through the vagina: the menstrual period. After this, the whole process of maturation and rejection begins again, until the supply of eggs is exhausted and the menopausal transition begins.
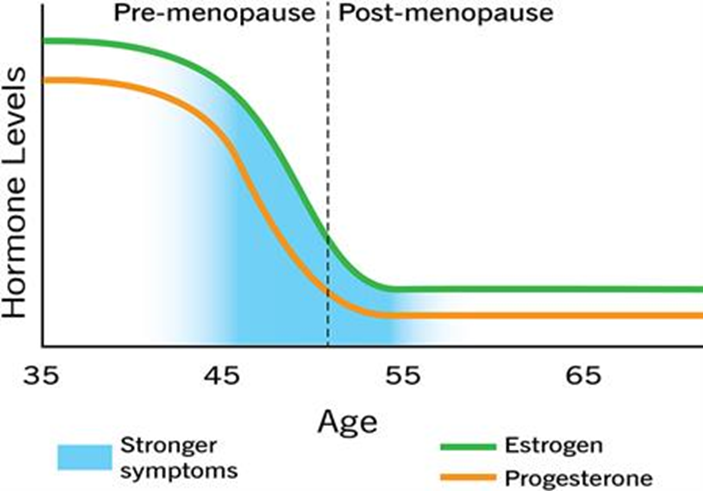
Menopause can be seen as a kind of reverse puberty. During puberty, the ovaries are activated and start producing the sex hormones estrogen and progesterone, after which an egg is released every month. The fertile period begins. During the menopause, the activity of the ovaries decreases. Because the stock of eggs in the ovaries is almost exhausted, the ovaries will produce fewer and fewer hormones, which means that an egg can no longer mature every month. Changes in the menstrual cycle are therefore usually the first sign of menopause. The periods between bleeds may become shorter or longer, and the bleeding may become more or less intense. This differs per person. The menopause has started, despite the fact that at that moment one does not have to suffer from menopausal complaints such as hot flashes. On average, the menopause period for a woman starts between her 45th and 55th year of life. Cycle changes begin on average four years before the last menstrual period. After the last menstrual period, complaints can persist for an average of five to seven years, sometimes up to ten years. It is a process of biological changes in which the sex hormones play an important role.
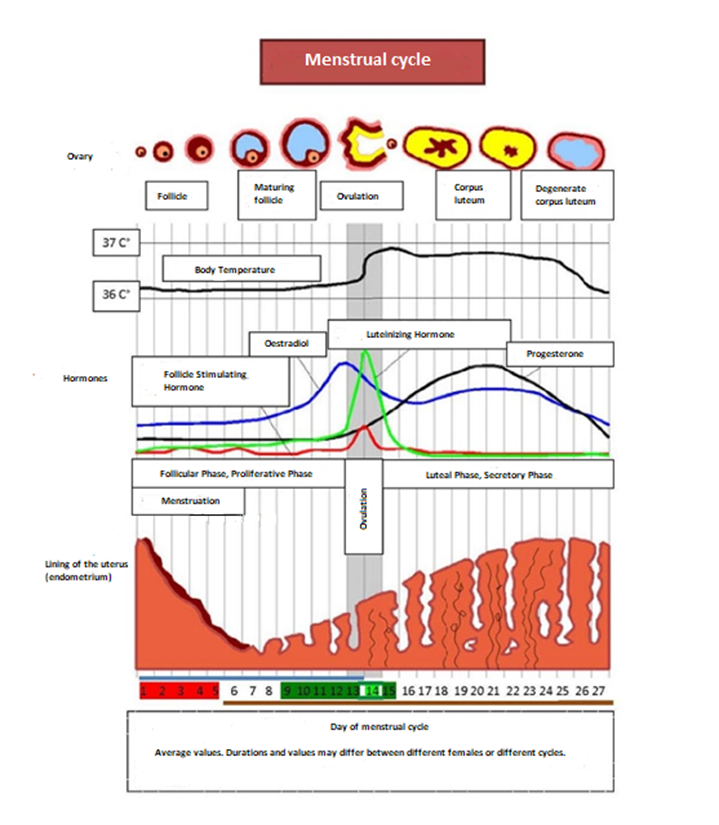
Bron: wikipedia.org/wiki/Bestand:MenstrualCycle
1.3 What is the menopause?
The menopause is the moment of the last menstruation. Due to, for example medical treatments for cancer, menstrual periods can stop immediately. Depending on the treatment, this can be temporary or permanent. In the spontaneous menopause, it takes an average of four years before the menstrual period stops permanently. This means that, even though you are still menstruating, you can already be in the menopause transition. Cycle changes are the result of progesterone deficiency. Often the cycle will be shorter initially and as you get closer to menopausal age, periods will be skipped. The last menstrual period is called menopause. So the menopause itself is only one moment. You can only determine this moment afterwards, when the menstrual period has been missed for one year. Postmenopause begins after menopause. The period before and after the last menstrual period is called the menopause. The fact that the last menstrual period has taken place does not mean that the complaints have been resolved; Menopausal symptoms such as hot flashes and sweating attacks are the result of estrogen deficiency and can persist for five to ten years after menopause. This also applies to women who have skipped the period of irregular periods due to medical treatment and who have entered the menopause abruptly.
The age at which a woman menstruates for the last time is influenced by several factors. The age at which your mother went through menopause can be an indication of your own menopause. Smoking advances the menopause by about two years. In the Netherlands, the average age at which women last menstruate is 51 years old.
Bron: Cleveland Clinic, 2019
|
Need to know more?
Do you want to know more about the period of menopausal transition? Visit www.thuisarts.nl/overgang.
Do you want to know more about guidelines on the period of menopausal transition? Visit one of the following websites:
https://richtlijnen.nhg.org/standaarden/de-overgang or https://richtlijnendatabase.nl/richtlijn/management_rondom_menopauze/behandelingen_bij_overgangsklachten.html.
2 The menopausal transition
The period of menopausal transition is a process that all women have to deal with sooner or later. The menopausal transition can be very drastic, especially if it happens to you unexpectedly.
You do not have to worry too much about what might happen as a result of the menopausal transition. Menopausal symptoms diminish and disappear over time. Moreover, you do not have to get (severe) menopausal symptoms. This varies greatly from woman to woman. There is much that can be done against menopausal complaints.
A list of possible menopausal complaints can come across as very negative, especially if they are described in a medical way. You may not be in the mood to read this list of menopausal symptoms. The menopausal symptoms may also not apply in your situation. You do not have to experience all these complaints either. You can then skip this chapter or look at it later and read only certain complaints. See chapter 3 Menopausal symptoms and lifestyle and/or treatment. What can I do about menopausal symptoms
2.1 What are the consequences of the menopausal transition?
Around the age of 50, the egg supply may have become so low that no more egg follicles grow and ovulation no longer takes place. Menstruation has stopped and the fertile phase of life has come to an end. Menopausal symptoms can arise if the body hardly produces the hormones estradiol (the main estrogen) and progesterone. Due to the changes in hormones during the menopause, it can happen that you are not feeling well. The reduction in estrogen production almost always causes complaints: 80% percent of women suffer from this. One in three of this group of women has such serious complaints that daily functioning is seriously disrupted.
It is good to remember that not every woman has the same complaints, but that these hormonal changes in the body almost always affect a woman's health. Menopause can also cause health problems in the long term. The consequences and complaints of the menopausal transition are often underestimated by those around you and seen as a phase that you have to go through. It is good to discuss your feelings in order to gain more understanding for menopausal complaints.
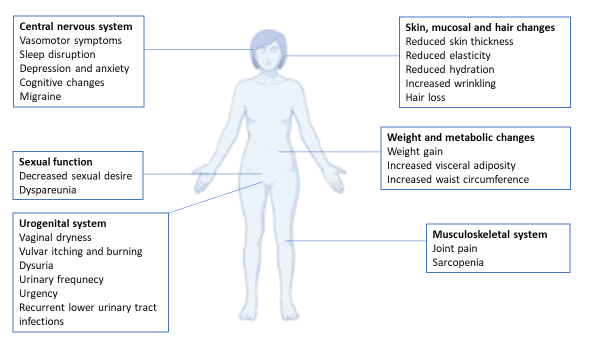
2.2 Which menopausal complaints may occur?
The most common complaints during the menopause are irregular periods, hot flashes and night sweats, vaginal dryness, pain during intercourse and problems with urination. These complaints are directly caused by the fluctuations in the amount of estrogen in the blood and are called 'typical menopausal complaints'. Atypical complaints are complaints that are not related to the menopause, but are often mentioned by women. For example, mood swings, irritability, dry skin and mucous membranes, pain during intercourse, lack of sex drive, fatigue or painful joints. Hormone treatment can be useful in severe menopausal symptoms.
The menstruation changes
Although you still have your period, the menopause may have already started. Irregular periods are the first signs of the menopause. The periods come shorter or longer after each other, become more intense (with blood clots) or less intense. Complaints that can go along with menstruation (abdominal pain, back pain) can occur for the first time, become worse or less than you were used to.
Hot flashes and night sweats
Hot flashes and night sweats are the most common menopausal symptoms. You can get hot flashes while you are still menstruating. You may suddenly become red in the face, become very hot and perspire profusely; it overtakes you during the day, but also at night. A hot flash usually lasts three to five minutes. Sometimes they come a few times a week, but sometimes more than twenty times a day.
It varies per woman how much she suffers from hot flashes. Some women suffer so much that they cannot continue with their activities. Hot flashes can be very annoying when you are at work or in a public place.
Insomnia and fatigue
Insomnia or light sleep and fatigue are common and can interfere with your daily life. Women who wake up at night drenched in sweat often sleep badly. Due to this insomnia, they often feel tired or gloomy during the day and energy loss occurs if these complaints persist for months or years. You may find that you are more tired during the day even if your sleep is not affected.
Vaginal complaints
Due to the decrease in oestrogens, the lining of the vagina gradually becomes thinner and drier. Also, the vaginal discharge is less. Many women suffer from itching and a burning sensation in the vagina and labia, or when urinating. The vaginal mucosa becomes fragile and intercourse can be painful and the bladder becomes more susceptible to infection.
Complaints of the urinary tract
With age, the pelvic floor muscles and the supporting tissues relax, allowing the bladder to sag slightly. Because the mucous membranes of the urinary tract become thinner, bladder infections can develop earlier. Together, this can result in the urine being unable to be held for as long as needed or urine being lost when coughing, sneezing or exercising.
Sexual complaints
With age, the blood flow to the genitals decreases. As a result it sometimes takes a little longer for women (and men) to start the physical sexual response. To get aroused properly, more time and more direct stimulation of the genitals is needed.
Hot flashes, night sweats, poor sleep and psychological complaints can also significantly influence the sex drive. A small proportion of women develop a testosterone deficiency during the period of menopausal transition, which can reduce the need for sex. This can occur in women who have had their ovaries removed. Of course, more factors can be of influence and it does not always have to be just the menopausal transition.
Fertility
Due to the menopause, the ovaries stop working and the fertile period has come to an end. It is no longer possible to become pregnant with your own eggs.
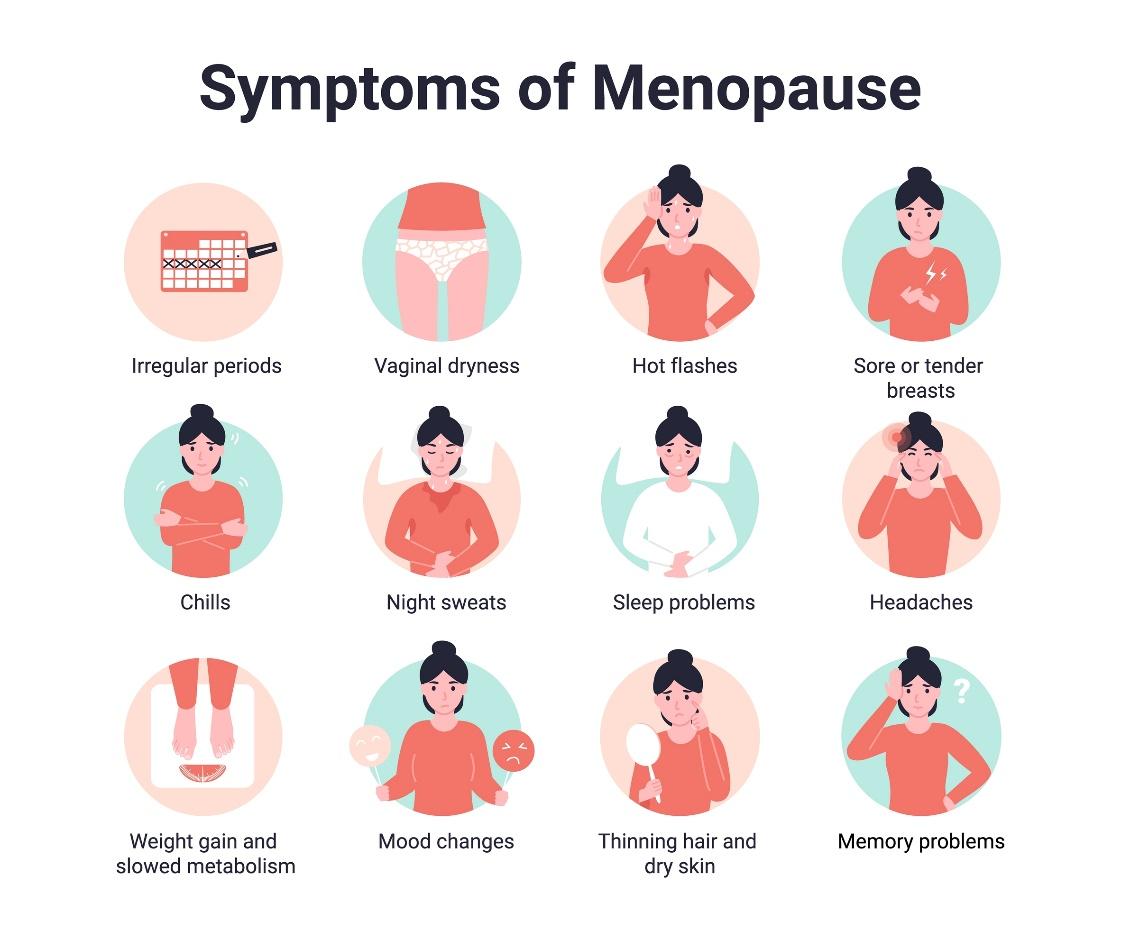
2.3 What other complaints are common in the years of menopausal transition?
Complaints that often occur during the menopausal transition, but are not related to the changes in the hormones, are called 'non-typical' menopausal symptoms.
Physical complaints
The menopausal transition leads to a decrease in collagen resulting in skin changes. The skin may become drier and less elastic; wrinkles may appear. Because less tear fluid and saliva is produced, the eyes and mouth can become drier. Hormonal changes can cause hair to gradually thin.
Many women suffer from muscle and joint pain. Stiffness of joints (hands and feet) can occur and give a painful feeling.
You may store more fat in the abdominal region and experience weight gain.
These changes in the body and appearance are not (only) the result of hormonal changes, but also occur with age.
Headaches can also develop during the menopausal transitional years, or migraines can get worse. In the years after menopause, headaches or migraines decrease if they were related to the menstrual cycle.
Psychological complaints
Not only physical, but also psychological complaints can occur. Estrogen also plays an important role in the brain. Due to the varying amount of hormones, you can suffer from mood swings, irritability, depression, forgetfulness and a reduced ability to concentrate. It is possible that you no longer feel like yourself, for example because you are irritable, sad or overtired and have less desire to do something. Mental complaints can also occur without changes in menstruation.
Of course, in addition to hormones, other factors may also play a role. Stress is a major cause of psychological complaints. Past depression or negative and impactful events from the past increase the risk of depression. The feeling of getting older, children who leave or parents who are in poorer health can also cause negative feelings.
Psychological complaints can be experienced as very severe and can make women insecure. It sometimes feels a bit personal to share this with others. At the same time, it can have a lot of influence on how one feels and behaves. Shame can also play a role in emotional reactions or hot flashes. Women may find that they have trouble with remembering things and are less attentive because they forget important things.
Bron: Nat Rev Endocrinol. 2018 Apr;14(4):199-215
2.4 Menopause and contraception
If you're over 45 and have not had a period for six months, most women's chances of pregnancy are virtually nil, but not impossible. Talk to your doctor about whether you still need contraception. If this is not the case and you are experiencing menopausal symptoms, there may be other options that are more suitable for treating them.
If you take the contraceptive pill, you usually do not know whether you are in the menopausal transitional phase. If you experience hot flashes or other menopausal symptoms during the stop week (the week that you do not take it), this may be an indication that you are already in the menopause. It is unclear when the menopause has been reached for women who use a hormonal IUD and do not have vaginal bleeding as a result. A hormonal IUD is intended for contraception or treatment of menopausal cycle or bleeding problems, but is not a treatment for hot flashes or sweating attacks. For this, if necessary, treatment with estradiol is prescribed with the hormonal IUD.
The general advice to stop using contraception is:
- with hormonal contraception at the age of 52 years
- with non-hormonal methods 1 year after the last menstrual period

2.5 What are consequences of the menopausal transition - the long-term?
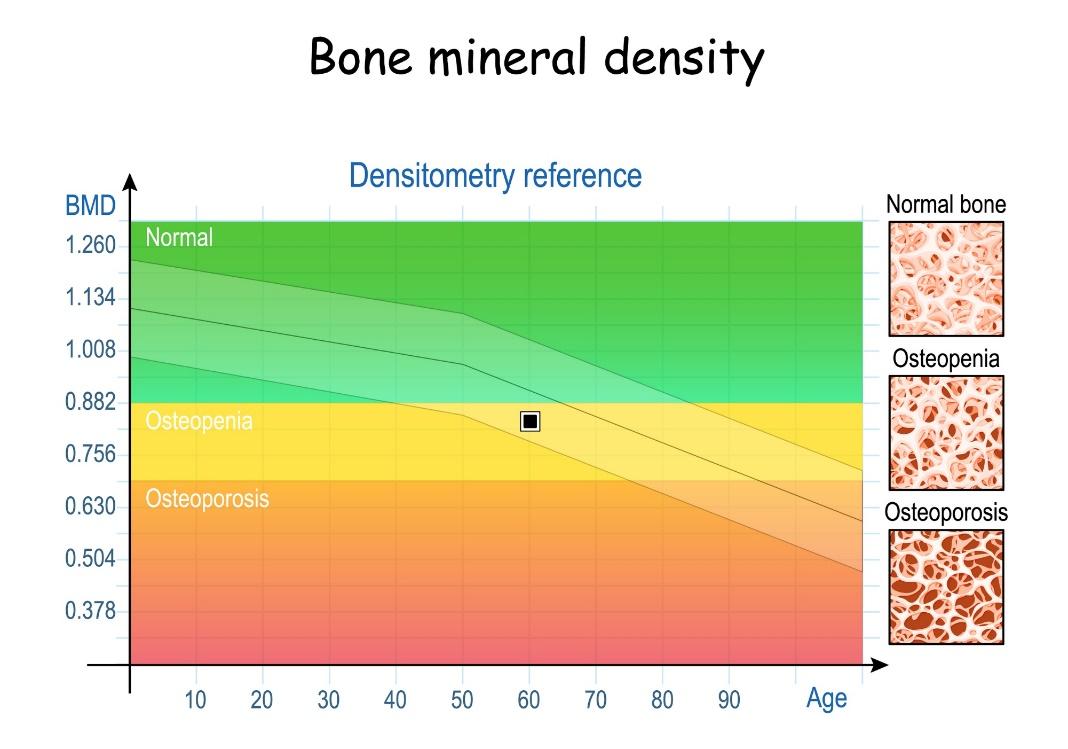
In the long run, bone loss can occur and the risk of cardiovascular diseases increases slightly; the risk of breast cancer is generally reduced in women who have entered the menopause because the estrogen exposure is less. A healthy lifestyle is important to reduce the symptoms of menopause and to minimize the risk of osteoporosis and cardiovascular diseases. Medicines can help with osteoporosis and cardiovascular diseases.
Bone decalcification (osteoporosis)
The hormone estradiol plays an important role in bone building. To get an impression of how the bones are constructed, one can measure the bone mineral density. If the bones contain enough calcium and you start taking medicines with female hormones, then further monitoring is unnecessary. If you cannot or do not want to use hormones, the measurement can be repeated after five years. If the bones have too little bone density (osteoporosis), treatment can be given, usually with bisphosphonates.
Heart and vascular disease
Women who enter menopause early have a slightly higher risk of cardiovascular disease. Other risk factors for cardiovascular diseases are genetic predisposition, unhealthy lifestyle such as smoking, unhealthy diet and little exercise, obesity, high blood pressure, high cholesterol and diabetes.
Dementia
Sex hormones are very important for the function of the brain. Dementia is much more common in women than men, but it is not yet clear whether there is a link with low hormone levels.
Need to know more?
Do you want to know more about the menopausal transition? Then visit the website www.thuisarts.nl/overgang.
For more information about osteoporosis, see the website of the osteoporosis association osteoporosevereniging.nl.
Risk factors for cardiovascular diseases are described on the website of the heart foundation hartstichting.nl/risicofactoren.
3. Menopausal symptoms and lifestyle and/or treatment
Menopausal symptoms require a personalized approach and guidance. You can do a lot yourself to be and stay healthy. It can be a search for the best way to deal with the menopause, but there are often solutions to feel good during and after the menopause and to age healthy.
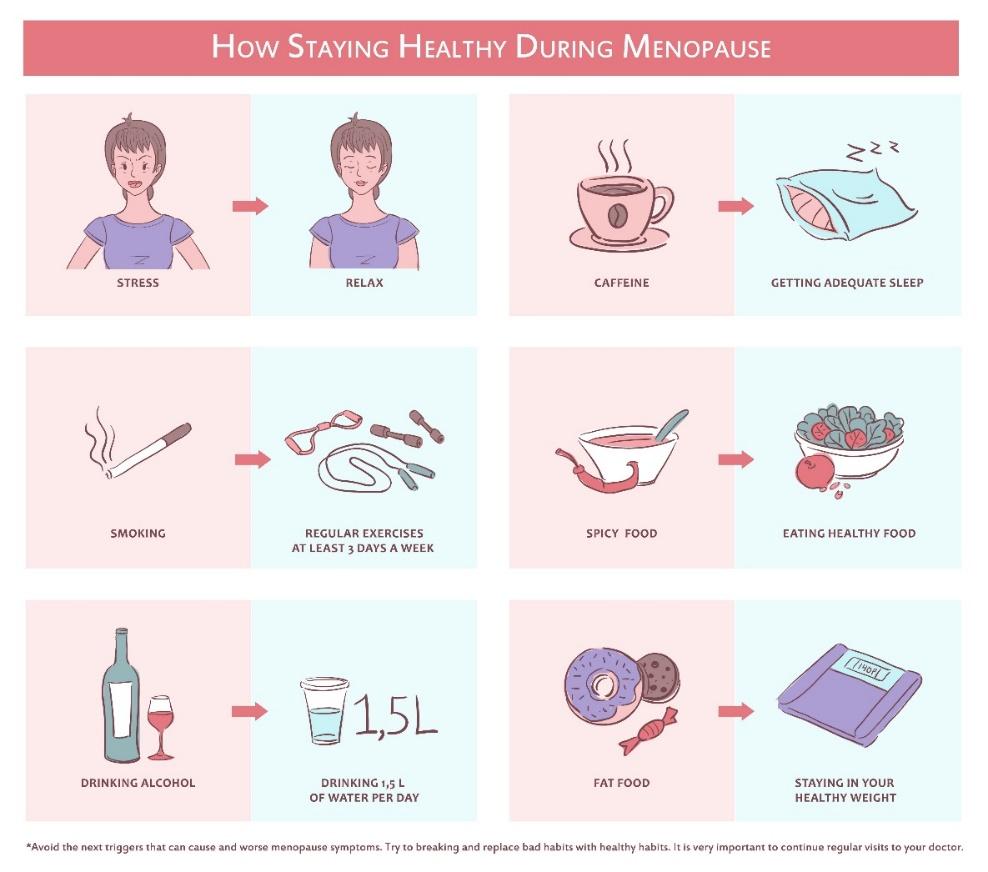
3.1 What can I do about menopausal symptoms?
Menopause is a natural process that every woman has to deal with in her life. An unhealthy lifestyle, such as unhealthy food and drink and little exercise, can significantly worsen menopausal symptoms. It can therefore help to take good care of yourself during the menopausal transition.
Lifestyle
A healthy lifestyle is the most important way to reduce menopausal symptoms, to minimize the risk of osteoporosis and cardiovascular disease and to slow down the process of aging:
- do not smoke
- healthy food
- little or no alcohol
- sufficient exercise
- healthy weight
- enough sleep
- prevention of stress
Women who smoke reach the menopausal age earlier and often suffer more from menopausal symptoms than women who do not smoke. A varied diet is important with lots of vegetables and as little saturated fats and added sugar as possible. Healthy exercise involves half an hour of moderately intensive physical activity at least five days a week. A healthy weight is based on a BMI between 18 and 25 (kg/height2). In the case of overweight, weight loss in the menopausal years can reduce hot flashes, because the adipose tissue prevents the ability to lose heat quickly. If your waist circumference in women is 88 cm or more and your BMI is 25 or more, your risk of cardiovascular disease increases. Other risk factors for cardiovascular disease include elevated blood pressure, elevated cholesterol or glucose.
It is important that you consume enough calcium (1000-1200 mg per day): four dairy or cheese products per day. If you have little or no dietary calcium (< 2 diary or cheese products per day), you can take calcium tablets (1000 mg per day) and vitamin D3 (20 micrograms per day), which you can buy at the drugstore or get a prescription from your doctor. Exercise that puts stress on the bones stimulates the production of bone; walking (including walking) helps against osteoporosis, swimming does not. Good exercise is also important for fitness and maintenance of muscle mass, however (extra) exercise does not help to combat hot flashes.
For hot flashes and perspiration attacks it is useful to:
- avoid hot drinks, caffeine, spicy food, sugars, alcohol
- wear clothing in layers and choose airy and natural fabrics such as cotton, silk or wool
- put a cool scarf or cool pack around your neck
- use a plant sprayer
- use a fan
- use several thin blankets made of natural material at night so that you can combine and alternate
- ensure a well-ventilated bedroom
- reduce stress
Menopause and sex life
Sexuality plays a major role in the lives of young women and the menopause is a phase of life in which a new balance can also be found in the field of sexuality. A healthy sex life contributes to a good quality of life. It is normal for more time and direct sexual stimulation to be required to become aroused. The moisture in the vagina is dependent on sexual stimulation and with relaxation of the pelvic floor muscles you can have painless intercourse.
Discuss vaginal complaints with your partner. Sometimes caution, taking extra time with foreplay or a vaginal moisturizing gel, capsule or lubricant can help. Your (GP) doctor or a sexologist can also offer help if you do not agree with your partner.
3.2 What can I expect from self-care products?
There are all kinds of products available for the menopause, such as herbal remedies or nutritional supplements. These products are without prescription available at the pharmacy or drugstore. However, make sure to receive good advice; not all these products have been shown to have a proven effect on menopausal complaints. (Chinese) herbal therapy is not effective for hot flashes or perspiration attacks. Studies show that dietary supplements containing plant estrogens (phytoestrogens), such as isoflavones in soy or red clover, or black cohosh extract (cimicifuga racemosa) slightly decrease the frequency of hot flashes, but no reduction in night sweats. Due to sub-optimal quality of studies and lack of long-term safety data, dietary supplements are not recommended in women with a history of hormone-sensitive cancer.
The exact composition of dietary supplements is often insufficiently known and there is a risk of overdose. Some products can actually have a negative effect on health. You should therefore seek advice from your GP, gynaecologist or menopausal nurse consultant.
If you experience discomfort from the menopause, it is advisable to discuss this with your doctor. Menopausal complaints can be treated well and you do not have to ignore them. Your GP can treat you or refer you to a gynaecologist who specializes in the menopause. In more and more Dutch hospitals there are special consultation hours for the menopause at the department of gynaecology. This requires a referral from the GP. You can also make an appointment yourself with a nurse, specialized in the menopause, via the association for nursing menopause consultants (overgangsconsulente.com).
Not all complaints that occur in the menopausal years are related to changes in the female sex hormones. When hot flashes, excessive sweating or agitation occur, it is also important to exclude other causes. For example, high blood pressure can imitate menopausal symptoms. Women who have thyroid disease may suffer from heat intolerance. Medicines can cause facial flushing, hot flashes or excessive sweating as a side effect.
3.3 What is a possible hormonal treatment for menopausal symptoms?
Medicines with female hormones can sometimes be useful for severe menopausal symptoms and they can also help with osteoporosis and (prevention of) cardiovascular diseases.
It is important that you discuss your complaints with a healthcare provider with a special focus on menopausal transition, in order to receive the proper treatment.
Every woman experiences the menopause in a different manner. You may be lucky and not experience many menopausal symptoms or you may have severe menopausal symptoms for years. An early menopause does not make the treatment of menopausal complaints more difficult.
One reason to use medicines with female hormones is serious menopausal symptoms at a (very) young age and/or to protect against osteoporosis. Medicines in the form of female hormones or the contraceptive pill can reduce or eliminate menopausal symptoms. You must weigh this advantage against the disadvantage of any side effects (breakthrough bleeding) and the increase in the risk of breast cancer with long-term use (after the 51st year of life). Hormonal contraceptive pills are not registered and researched for the treatment of menopausal symptoms. The dosage and type of estrogen and progestogen are more effective, because ovulation must be inhibited. In hormone replacement therapy for the treatment of menopausal symptoms, the hormones are based on low-dose endogenous estradiol and progesterone. The lower dosage and use of pure hormones during the menopause is important, because the risks of cardiovascular disease, thrombosis and breast cancer are higher at an older than at a younger age. Comparative research between hormonal contraceptive preparations and hormone replacement therapy is lacking. Hormone replacement therapy does not inhibit ovulation.
If you suffer from menopausal symptoms, it is advisable to discuss with your practitioner which treatment is most suitable for you. Your doctor may suggest taking estrogen and progesterone tablets. It is also possible to use an estradiol patch, spray or gel in combination with progesterone tablets. If you still need contraception, the doctor sometimes suggests using a hormonal IUD along with estrogen tablets or patches, or may the pill may be prescribed. You can discuss possible other non-hormonal treatments with your doctor if you cannot or do not want to use hormones.
Hormone replacement therapy has been proven to be most effective against symptoms caused by estrogen deficiency, such as hot flashes, poor sleep, irritability, and other complaints mentioned earlier in this flyer.
Hormone replacement therapy for the menopause comes in different forms and doses. Some types of therapy cause regular bleeding, while others do not effect it. Hormone replacement therapy does not delay the menopausal transition, but can help you through the period of menopausal transition.
Because hormones, like any drug, have advantages and dis-advantages, it is important to discuss with your doctor whether the benefits outweigh the harms, and whether it is still necessary to continue taking them. In some cases, hormones can cause side effects in the beginning, such as headaches, irregular bleeding or breast tenderness. These complaints may reduce after a few weeks, when your body has become accustomed to the new hormone balance.
Learn more about hormones prescribed during the period of menopausal transition.
|
Hormone |
Application |
Brand name |
|
|
Type of Estrogen |
Menopausal complaints |
Prevention osteoporosis |
|
|
Estradiol tablet |
+ |
+ |
Estradiol Zumenon |
|
Estradiol patch |
+ |
+ |
Systen Estradiol |
|
Estradiol gel |
+ |
+ |
Oestrogel |
|
Estradiol spray |
+ |
- |
Lenzetto |
Progestin will be combined with estrogen if the uterus is not removed
|
Type of progestin |
Brand name |
|
Progesteron capsule |
Utrogestan |
|
Dydrogesteron tablet |
Duphaston |
|
Levonorgestrel IUD |
Mirena |
Other not combined with estrogen
|
Tibolon |
Livial |
Estrogen and progestin combination tablets if the uterus is not removed
Hormone supplementation without vaginal bleeding
|
Hormone |
Application |
Brand name |
|
|
Menopausal complaints |
Prevention osteoporosis |
||
|
Estradiol+dydrogesteron 0,5 mg/2,5 mg |
+ |
- |
Femoston continu 0,5/2,5 |
|
Estradiol+dydrogesteron 1 mg/5 mg |
+ |
+ |
Femoston continu 1/5 |
|
Estradiol+progesteron 1 mg/100 mg |
+ |
+ |
Bijuva |
|
Estradiol+drospirenon 1 mg/2 mg |
+ |
+ |
Paosonelle |
Hormone supplementation with artificial cycle, vaginal bleeding for a few days after about 28 days
|
Hormone |
Application |
Brand name |
|
|
Menopausal complaints |
Prevention osteoporosis |
||
|
Estradiol+dydrogesteron 1 mg/10 mg 14 days every 28 days |
+ |
+ |
Femoston 1/10 |
|
Estradiol+dydrogesteron 2 mg/10 mg 14 days every 28 days |
+ |
+ |
Femoston 2/10 |
Hormone vaginal
|
Hormone |
Application |
Brand name |
|
Vaginal dryness |
||
|
Estriol capsule 0,5 mg |
+ |
Synapause ovule |
|
Estriol crème 1mg/g |
+ |
Synapause crème |
|
Estradiol tablet 10 mcg |
+ |
Vagifem or Vagirux |
For information, see the following website College voor Beoordeling van Geneesmiddelen (the Dutch MEB, Medicines Evaluation Board).
|
|
Gel |
|
Patch |
3.4 What are the risks of hormone treatment for women in the menopause?
Not everyone is allowed to use hormones at the menopausal age. In particular, women who are prone to thrombosis or who have or have had breast cancer are not advised to use hormones. In that case, you can discuss with the doctor whether there are other options.
Thrombosis
If you previously have had a thrombosis (in a vein), it is advisable to restrain the use of hormones. The hormone estrogen increases the risk of thrombosis. There are also other risk factors for thrombosis, including older age, surgery, cancer, use of the pill, smoking or overweight. When using hormones against menopausal symptoms, women can choose to use estradiol through the skin instead of tablets. There is no increased risk of thrombosis when a low dose of estradiol is administered via the skin.
Breast cancer
The risk of breast cancer is determined, among other things, by the number of years that the breasts have been exposed to female hormones. It does not matter whether these female hormones are produced by the body or taken 'from the outside'. Women with an early menopause lack most of the normal hormone production and therefore may have a lower risk of breast cancer. If you have an early menopause and you start using hormones until you are 51, the risk of breast cancer increases again. This chance is probably similar to that of women who have continued to menstruate or use hormonal contraception until the age of 51.
It is important to know that taking hormones for more than five years while you are over 50 may slightly increase your risk of developing breast cancer. The risk of breast cancer is also increased by smoking, being overweight or drinking alcohol. Because the risk depends on the type of hormones you use, it is recommended that you always use the lowest possible dose and preferably use hormones that are closest to the body's own hormones. A low dose of the body's own hormones (estradiol and progesterone) does not increase the risk when used for up to five years.
Other risk factors for breast cancer are: the first menstrual period at a young age, the last menstrual period at a later age (menopause), the first pregnancy at a later age (over 30 years), having no or few pregnancies, no or short breastfeeding, long-term use ( more than 5 years) of hormonal contraception (incl. hormone coil) or hormone preparations for menopausal symptoms, more alcohol, more smoking, more weight gain in adulthood, less exercise, earlier (a pre-stage of) breast cancer, radiation of the chest at a young age, certain genetic variants .
|
Age |
The chance of breast cancer being detected |
|
30-39 years |
0,6 out of 1000 |
|
40-49 years |
1,9 out of 1000 |
|
50-59 years |
2,9 out of 1000 |
|
60-69 years |
3,6 out of 1000 |
|
70-79 years |
3,3 out of 1000 |
|
80 years or older |
3,7 out of 1000 |
Warnings and precautions, risks and side effects are mentioned in the package leaflets of hormone preparations. If you are concerned about the safety of hormones, discuss this with your healthcare professional. The hormones for the treatment of menopausal symptoms are lower dosed and purer than the hormones used as contraception.
Hormones for vaginal complaints
If you only suffer from a sensitive vagina or a sore feeling in the vagina, the doctor can recommend a vaginal cream, ovule or tablet with estrogen, which can help against these complaints. These hormones only work in the vagina and are hardly absorbed into the body, so they rarely cause side effects. The practitioner will personally coordinate the use of this therapy with you.
3.5 Which non-hormonal treatment can be used?
Tablets without female hormones (clonidine, certain antidepressants (serotonin reuptake inhibitors) or gabapentin) can reduce hot flashes by up to 50%. This medication can be advised in women who cannot or do not want to use hormones.
- Clonidine can be used in menopausal complaints. Side effects may include dry mouth, dizziness, constipation, low blood pressure and drowsiness). Treatment with clonidine should not be stopped abruptly, but withdrawn slowly.
- Fezolinetant is a non-hormonal medicine used in menopausal women with moderate-to-severe hot flushes or night sweats. Fezolinetant restores the balance between a protein called neurokinin B and estrogen in the brain’s temperature control center. Possible side effects are diarrhea, difficulty sleeping or increase in levels of certain liver enzymes.
- Antidepressants are not registered for the indication menopausal symptoms, but can have a beneficial effect and help women who have a low mood. Examples are venlafaxine, paroxetine and citalopram. Side effects may include nausea, dizziness, drowsiness or insomnia, loss of libido and headache. It is recommended that you gradually taper off antidepressants. Paroxetine should not be combined with tamoxifen (breast cancer treatment).
- Gabapentin is not registered for the indication menopausal complaints. This medicine is used, among other things, in epilepsy. Gabapentin is used in the evening and can help women who have disturbed sleep due to night sweats. Side effects may include dizziness, drowsiness and tiredness.
- Oxybutynin is not registered for menopausal complaints. This is used for an overactive bladder. Oxybutynin has been studied to a limited extent in menopausal complaints during 12 weeks. Further studies are needed to compare its efficacy with other drugs. Dry mouth is the most common side effect of oxybutynin.
- Self-care products can be bought without a prescription at a drugstore, pharmacy, via the internet, etc. If you want to use self-care products, it is wise to discuss this with your doctor. Products may have an estrogenic effect or a placebo effect.
- Cognitive behavioral therapy is an effective treatment for menopausal complaints. Cognitive behavioral therapy is a type of psychotherapy, in which you learn to better deal with hot flashes, night sweats, sleeping problems and stress during the menopausal transition years. It means that changes are offered in your thinking and behavior about the menopausal symptoms and you are stimulated to practice relaxation and abdominal breathing.
Medicines against osteoporosis
Two types of drugs can be used for low bone density or accelerated bone breakdown:
- For prevention of osteoporosis: Use of drugs containing female hormones (as described above).
- In osteoporosis: Use of specific bone-strengthening agents (usually bisphosphonates).
You can discuss these options with your doctor, gynaecologist or internist.
Need to know more?
The menopausal transition is a period of great changes. It is important to consider what is happening in your body, so that you can find a good balance, stay healthy longer and still enjoy life to the full despite this troubled period.
You will receive this information in addition to the oral information given to you by the doctor/gynaecologist/nurse. In addition, we describe what you can expect when you have entered the menopause as a result of the treatment. Sometimes your doctor gives different information and/or advice than described herein. For example, because your situation is different or because there are recently new insights in this area. If you have any questions after reading this information, you can always discuss them with your attending physician/gynaecologist/nurse.
The Dutch Society for Obstetrics and Gynaecology (nvog.nl) is a professional association for gynaecologists. Although the NVOG is not a patient association, it does see it as its duty to provide patients and relatives with the necessary information. You can also go to the site of degynaecoloog.nl for information from the NVOG. In addition, there is an overview of links to relevant websites for patients.
For more information, see the Thuisarts.nl website
thuisarts.nl/seksuele-klachten-vrouwen
Would you like to know more about thrombosis? Then visit the website www.trombosestichting.nl.
For Combined Lifestyle Intervention (GLI) see RIVM: Loket gezond leven - GLI. The recognized Lifestyle Interventions that fall under the basic health insurance package can be found on www.loketgezondleven.nl.
For more information about risk factors, prevention and treatment of osteoporosis see the website of the osteoporosis association
osteoporosevereniging.nl/osteoporose/risicotest.
Auteur: M.M.A. Brood- van Zanten, arts endocrinologische gynaecologie
Engelse vertaling door Quality Concern
Bron overige afbeeldingen: Shutterstock

 Pills
Pills
 Spray
Spray