You have been diagnosed with (a suspicion of) a narrowing of the urethra, also called: a urethral stricture. This leaflet explains what this means, which examinations need to be carried out and what the possible treatment options are.
Urethral stricture
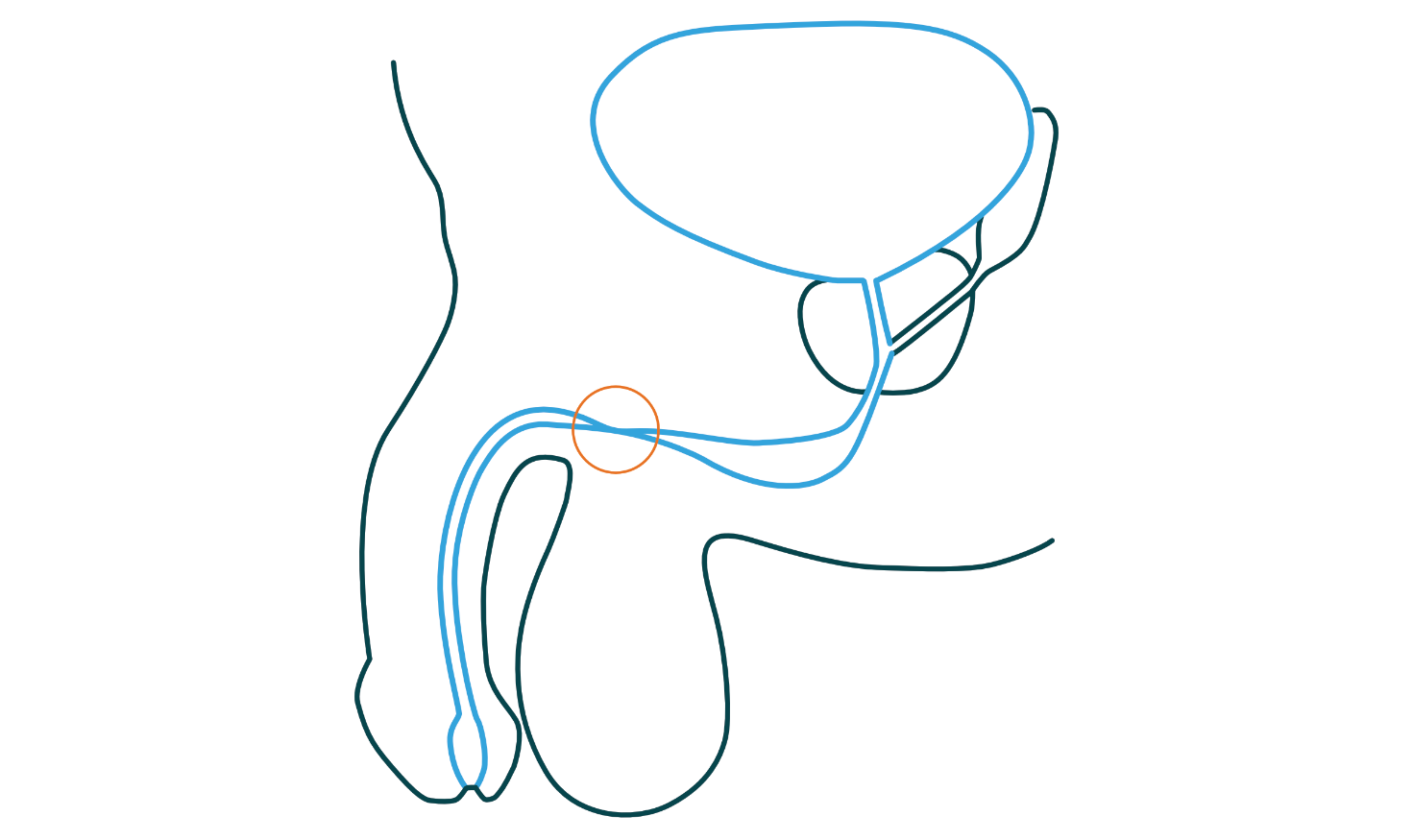
A urethral stricture, or a narrowing of the urethra, occurs in less than 1% of the population. The narrowing can be caused by: an infection, damage to the urethra due to an operation or catheter, family history or a combination.
A urethral stricture can occur anywhere in the urethra and varies from person to person in degree: from a long stricture to a narrow ring. It is important to first determine what the exact complaints are, where exactly the narrowing is located and how long it is. A number of questionnaires will therefore first be completed and an examination will be carried out to properly visualize the urethral stricture.
Diagnosis
To properly map out your complaints, the urologist will perform the following examinations.
Questionnaires
- IPSS: you complete this questionnaire so that the urologist or nurse specialist can get an idea of what exactly your complaints are.
- The micturition list: on this list you keep track of how much and how often you urinate in a day. Buy a measuring jug for this and measure the amount you urinate each time you go to the toilet. State the time and the amount on the micturition list.
Uroflowmetry (measurement of the urine stream) and residue determination
A flowmetry is a test in which you urinate on a special toilet. For this you must have the urge to urinate. The nurse will call you and show you the special toilet. The toilet measures how strong the urine stream is, how much you urinate and how long it takes. Immediately after urinating, the nurse will measure how much urine is left (residue) in the bladder. This is done with an ultrasound device and takes a few minutes.
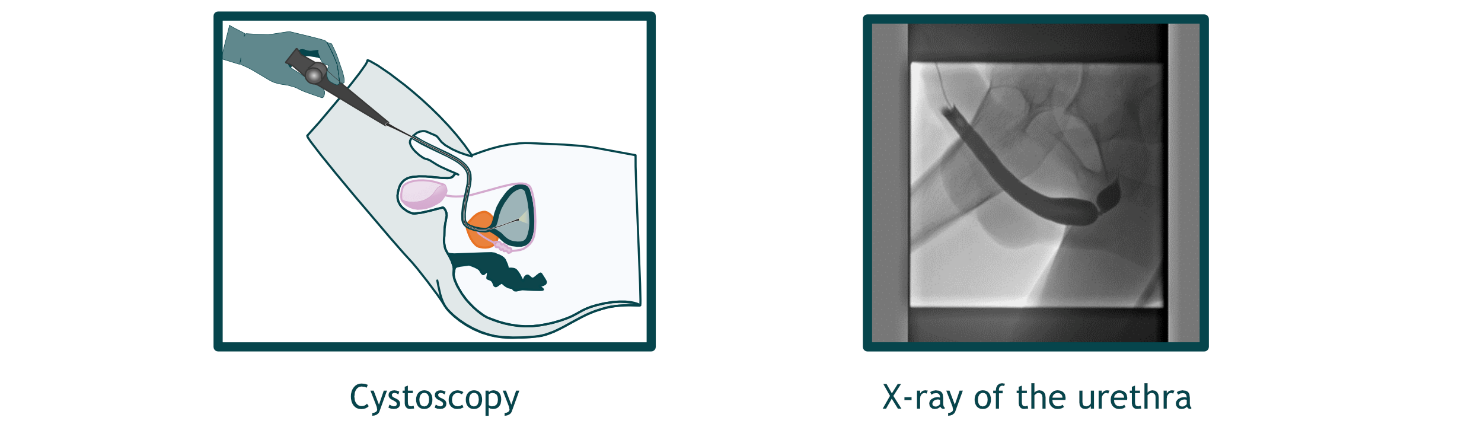
Cystoscopy
A cystoscopy is an endoscopic examination that takes place at the Urology department. A cystoscope is a tube that is inserted into the urethra. There is a camera on the end that the urologist can use to look into the urethra and bladder. The examination takes about 15 minutes. No special preparations are required for the cystoscopy.
X-ray examination (retrograde urethrogram)
A retrograde urethrogram is an X-ray taken by the urologist at the urology department. Contrast fluid is injected into the urethra, after which an X-ray is taken. The urologist can usually explain to you immediately what can be seen and what the best plan of action is.
Treatment
This brochure will provide general information about the treatment of a urethral stricture. Based on your symptoms and examinations, your urologist will draw up a treatment plan together with you. A number of options that are possible for urethral strictures are briefly explained below.
Non-surgical
- Do nothing for the time being
- Stretching the stricture with catheters: autodilation
- Stretching the stricture: balloon dilation
Surgical
- Cutting the stricture: urethrotomy
- Open surgery via the perineum: end-to-end urethroplasty
- Open surgery via the perineum: onlay urethroplasty
Non-surgical
Do nothing for the time being
Sometimes the best choice is to do nothing (for the time being), for example when the symptoms are not serious and the urologist estimates that there is little danger to the body. In that case, you will remain under supervision and can easily contact us if your symptoms worsen.

- No disadvantages of treatment

- No immediate solution
Stretching the stricture with catheters: self-dilation
Dilation means stretching the urethra. This is done by means of catheters that slowly widen the urethra. In general, this does not hurt because the diameter is slowly built up. The urologist will make a plan with you regarding how often this is necessary.

- Simple and safe
- Can be done at home

- No permanent solution
- Must be repeated (the frequency of this varies per person, sometimes once a day)
Surgical
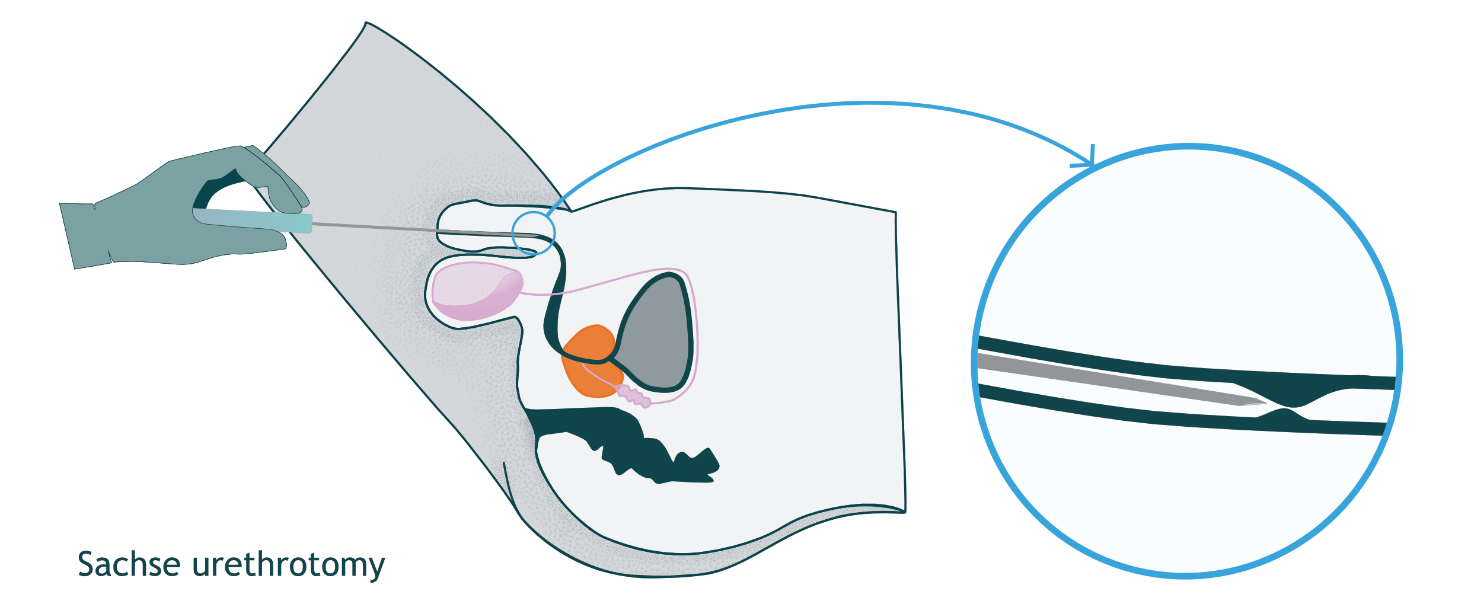
Incision of the urethra – urethrotomy
A urethrotomy is an operation via the urethra in which the stricture is cut. This is only possible when a stricture is short (shorter than 2 cm). A urethrotomy is performed under general anesthesia or a spinal injection.

- A relatively minor operation from which you recover quickly

- A 40% chance that the stricture will return
Open surgery: end-to-end or onlay urethroplasty
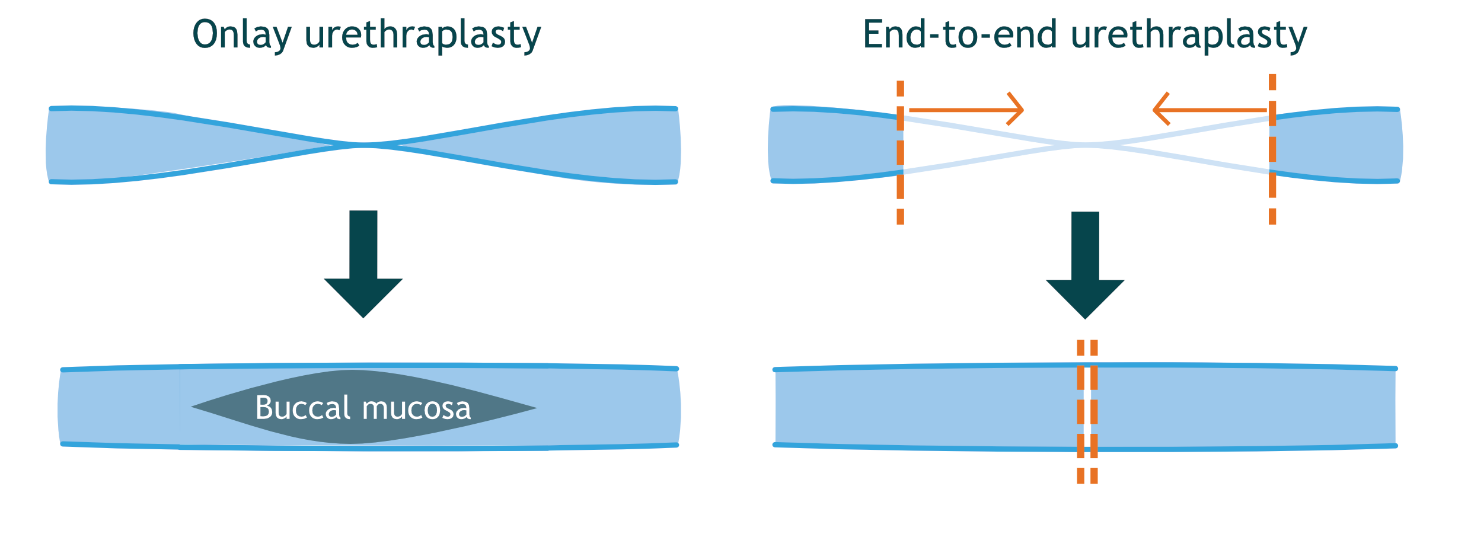
Urethroplasty is a collection of open operations on the urethra. The two most important forms are end-to-end and onlay urethroplasty. In both cases, the urethral stricture is reached via the perineum (the piece of skin between the scrotum and the anus). Below you can read what the difference is between the two types of urethroplasty. Afterwards, you will have a catheter for 2-3 weeks to give the urethra rest. This is removed at the outpatient clinic by the urologist.
After a urethroplasty, you will be monitored for another year. After the catheter has been removed, you will return to the outpatient clinic 3 more times over the course of 1 year to perform a uroflowmetry and to discuss how the recovery is going.
End-to-end urethroplasty
If the urethral stricture is short, this part of the urethra is removed. The ends of the urethra are then reattached. This makes the urethra slightly shorter.

- Permanent solution
- Chance of success 85-90%

- Relatively major surgery with longer recovery
- Indwelling catheter for 2-3 weeks
Onlay urethroplasty
If the urethral stricture is longer, or the tissue around a short stricture is not vital enough, buccal mucosa is used to widen the stricture. Buccal mucosa is a well-perfused tissue that resembles the lining of the urethra. Cutting away the buccal mucosa and inserting this tissue is done in one operation. The wound in the mouth generally heals within a few days.

- Permanent solution
- Chance of success 80-95%

- Relatively major operation with longer recovery
- Indwelling catheter for 2-3 weeks
- Wound in the mouth
Possible complications after surgery
- Recurrence of the narrowing
After surgery, you may experience a new narrowing in the urethra. The surgery can cause scar tissue to form that causes a new narrowing. Some men experience this shortly after surgery, others much later. Sometimes the narrowing keeps returning. In that case, the choice may be to stretch the urethra or to undergo a new surgery. - Numb, tingling sensation
Less than 10% of men experience a numb, tingling sensation at the site of their surgery. This always goes away, but it can last for several months. - Infection
With every surgery, there is a risk of infection. To minimize this risk, you will be given antibiotics before the surgery. - Postoperative bleeding
Postoperative bleeding is also a general risk with every surgery. - Incontinence
Incontinence is almost never the result of urethral surgery. However, some men do experience this temporarily. This is usually because urine suddenly flows more easily through the urethra. A catheter also temporarily weakens the sphincter. If this happens to you, it can be remedied with the help of exercises from a pelvic physiotherapist. - Erectile dysfunction
Urethral surgery does not affect erection and sexual life. Ejaculation can actually improve after the procedure. Approximately 5% of men still suffer from erectile dysfunction. This usually goes away on its own, although it can take up to six months. Temporary use of erection pills can be a solution. A visit to a sexologist can also help.
Rare complications
The following complications occur very rarely (less than 1%):
- Abnormal connection between the urethra and the skin (urethral fistula).
- Damage to the salivary gland when removing buccal mucosa for urethroplasty.
- Temporary taste disturbances.
- Long-term pain in the perineal area.
- Tight inside of the cheek due to the removal of mucosa.
- Nerve damage and blood flow problems in the lower legs due to long-term pressure in the calves while lying in leg supports.
Information
If you are worried or have questions about the diagnosis, examination or treatment, it is best to contact your healthcare provider by sending him or her a message via the My File environment.
You can contact us by telephone during the nursing consultation hours of the Urology outpatient clinic via 020 444 1103. The nursing consultation hours are from Monday to Friday from 8:30 to 9:30.
You can also visit our website: www.amsterdamumc.nl Specialismen Urologie
Finally
Amsterdam UMC is a university medical centre where medical specialists are trained. They independently hold consultations and assist with operations. As a result, it may happen that you have an appointment with your urologist and meet another doctor. This is an assistant in training to become a specialist (AIOS). He or she works independently, but always under the responsibility of your urologist. If you prefer to speak to your own urologist, you can indicate this when you make an appointment. We will try to take your wishes into account.
This brochure contains general information. It is intended as additional information in addition to the conversation with your treating physician.
