This brochure provides information about the ovaries, the reasons for removing one or both ovaries, and the method (keyhole surgery).
The uterus, fallopian tubes, and ovaries - general information
A normal uterus (uterus) is shaped and sized like a pear. At the wide top, two fallopian tubes (tubes) empty into the uterus. These thin, flexible tubes, 8 to 10 cm long, begin at the uterus and end at the ovaries. Normal ovaries are about 3 cm in size. The uterus, fallopian tubes, and ovaries are not loose in the abdomen but are attached to the pelvis with blood vessels and connective tissue bands. The ovaries make hormones that build up the endometrium each month. The uterus is lined on the inside (uterine cavity) with this mucous membrane which, under the influence of hormones, is shed monthly through the cervix and vagina (menstruation). The hormones also contribute to the desire for sex (libido) and to keeping the vagina firm, supple and moist.
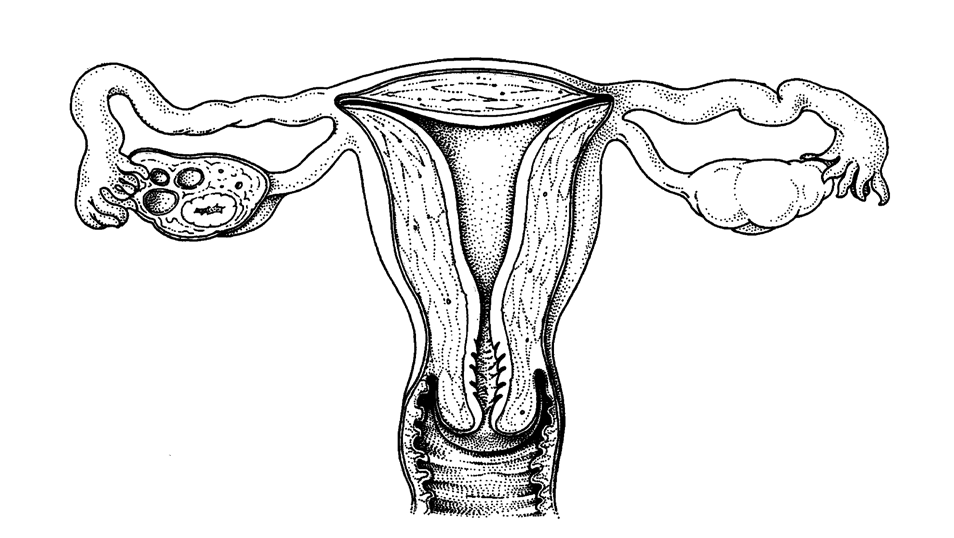
Uterus, fallopian tubes, and ovaries in cross-section
Reasons to remove an ovary (and fallopian tube)
- A cyst on the ovary
- An increased risk of ovarian cancer
A cyst on the ovary
The ovaries contain eggs and make hormones. In an ovary, a cyst can develop. The cyst may contain fluid (clear fluid, blood, mucus). It may also have hair, particles of bone, and sebum. Often, a cyst is harmless. It is usually not cancerous.
Increased risk of ovarian/egg cancer
You are at an increased risk for ovarian/ovarian cancer due to carrying a BRCA 1 or BRCA 2 gene mutation. It is also possible that you have a familial connection: two or more women in your family have ovarian cancer, but no genetic predisposition could be identified. Unfortunately, if you are genetically predisposed, there is no way to know if you will get ovarian cancer. In addition, ovarian cancer does not have a clear precursor, and early detection by screening is not possible. Therefore, the only effective measure you can take to prevent ovarian cancer is to have your ovaries and fallopian tubes removed as a precaution.
The operation
The procedure is performed through keyhole surgery (laparoscopy, see image). The operation is performed under general anesthesia by a gynecologist together with a trainee gynecologist.
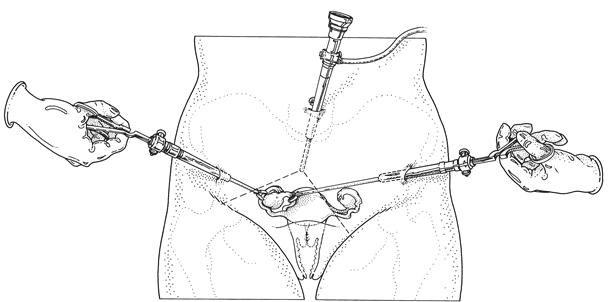
The gynecologist usually makes an incision of about 1 cm in the lower edge of the navel. That incision inserts a thin hollow tube into the abdominal cavity. The abdomen is first filled with carbon dioxide (CO2). This creates space in the abdomen to view the various organs. Then, the gynecologist inserts the viewing tube (laparoscope) into the abdomen and connects it to a video camera through the same tube. The uterus, fallopian tubes, and ovaries are thus visible on the screen. Then, small incisions are usually made in 2 other places, on the left and right side of the abdomen next to the hip bones. Through these, the surgical instruments are inserted. In total, the gynecologist will make 3 incisions, and sometimes a fourth is needed, which is then placed next to the navel or above the pubic bone. Sometimes an instrument is placed on the cervix through the vulva or inserted into the uterus to allow it to move. This may be the reason for vaginal bleeding after the procedure.
Next, the ovaries and fallopian tubes are detached from the uterus and pelvic wall. After these are detached, the ovaries and fallopian tubes are placed in a small bag brought out through the abdominal wall, through the same incision that the instruments went in.
Operational risks
Most laparoscopic (=looking tube) surgeries (95 percent) proceed without complications. However, the possible complications that can occur are discussed below:
- In about 2 percent of laparoscopic surgeries, a "normal" abdominal surgery (laparotomy) must still be performed through a larger incision (bikini incision). This is especially the case if you have had abdominal surgery before. Sometimes surgery using the laparoscopic method is not possible or safe. For example, in case of extensive adhesions after a previous abdominal disease or abdominal surgery(s). This is usually already known and discussed with you before laparoscopic surgery. Very sometimes, this becomes clear only during surgery. So please keep in mind that there is a very small chance that you will wake up with a larger incision than planned. Hospitalization and recovery will also take a little longer in this case.
- In very rare cases (less than 1 percent), the urinary tract or the intestines can be damaged during keyhole surgery. The consequences are usually visible during the operation; very rarely it becomes clear until you have been discharged from the hospital. You may experience more pain instead of less. In that case, you should call the hospital. These lesions are usually treatable, but they sometimes require another surgery, extra care, and recovery takes longer. If a lesion develops and is discovered during surgery, it is repaired immediately, usually through the viewing tube.
- Before surgery, a tube (catheter) is inserted into the bladder. As a result, there is a small chance that a bladder infection will develop. You will notice this by a burning sensation when urinating. This is troublesome and painful but treatable with an antibiotic.
In general, patients who do not smoke, or have quit smoking at least five weeks prior to surgery, are less likely to have complications from the procedure and anesthesia, especially to the respiratory tract.
Prior to the operation
After the gynecologist discusses the surgery with you, you will be placed on the waiting list for the surgery. The surgery scheduler will contact you to discuss a possible date for the surgery with you.
Beforehand, a doctor who administers anesthesia (anesthesiologist) conducts a preoperative screening through the preassessment clinic in the Department of Anesthesiology. This consists of a telephone or outpatient consultation. If necessary, a general physical examination, sometimes supplemented by blood tests, a lung X-ray, or a cardiac ultrasound (ECG), will be performed. Next, the anesthesiologist will discuss anesthesia with you. Only after you have been to the anesthesiologist can the surgery be scheduled. The surgery usually takes place during an inpatient day or through an outpatient clinic.
In principle, you can be discharged home the same day. However, depending on the severity of the procedure or when the operation ends, you will stay in the hospital from one night to several days. The gynecology care unit at the clinic of the Amsterdam UMC location AMC is located at G6Noord. The outside clinic is the Boerhaave Medisch Centrum, Dintelstraat 60 in Amsterdam, where surgery space is rented.
The day of surgery
You may not eat or drink anything for six hours prior to surgery. You may also not wear makeup or nail polish. A nurse will take you to a room where the operation clothes will be ready for you. The doctor who will operate on you will visit you beforehand to introduce themselves and ask if you have any questions. Then the nurse will take you to the operating room. There you will be asked to lie down on the operating table. Then the arrangements surrounding the operation will be briefly reviewed in your presence by the doctor who will be operating on you, the anesthesiologist, and the operating assistant. Next, you will receive an IV, usually at the top of your left hand. Through this drip, you will be administered the anesthetic and fluids. You will fall asleep and not notice anything until you wake up in the recovery room after surgery. Once you are under anesthesia, a catheter (tube) will be inserted into your bladder. Next, laparoscopy (keyhole surgery) is performed as discussed earlier. The surgery takes an average of 30-60 minutes. After the keyhole surgery, you will stay in the recovery room for a while, after which you will be taken back to the ward.
You may have a brief sore throat due to the tube inserted under anesthesia to ventilate you. As a result, you may experience some nausea and vomiting. The IV will remain in place until the nausea is gone and you can drink on your own. Usually, the nurse will remove the IV just before you go home. However, if the surgery takes place late in the afternoon, the IV may not be removed not until the next day. You will be given medication for pain and nausea after surgery. In addition to abdominal pain, some patients also experience shoulder pain caused by the carbon dioxide gas introduced during surgery and stimulates a nerve that runs through the diaphragm to the shoulders. This pain usually disappears after a day. If you have pain, you can use paracetamol for this, up to two tablets 4 times a day (maximum 1000 mg 4 times a day).
The gynecologist will visit you before you go home to tell you how the surgery went. If you are well awake, have urinated and eaten, or drunk something, you may go home. You may not drive yourself home after surgery. We also advise you not to be home alone the first night.
Recovery
In general, you should count on one to two weeks for recovery. During the first few days, you can generally take care of yourself, but not, for example, your family. Before you are admitted, it is advisable to make arrangements for the period after your discharge from the hospital. One of the advantages of laparoscopic surgery is a smoother recovery compared to "normal" abdominal surgery. However, for some women, this can also be a disadvantage. For those around you, these small incisions and quick discharge from the hospital may make it seem like you are hardly sick at all, so you will have less help and support at home than after a "normal" surgery with a larger incision. Even though you do not have a large abdominal wound, you may still have pain and feel weak. Depending on the severity of the surgery and the situation at home, you may need some help after returning home. Discuss this in advance with your family or community. If you work outside the home, you should generally expect to be absent for one to two weeks. Possible complications and your condition play a role here. You will often have abdominal pain, be more tired, and be able to cope with less than you might have expected. Your body tells you what you can and cannot handle. It is important to 'listen' to this, based on which you can gradually expand your activities.
To close the wound, one usually uses sutures that dissolve on their own. This takes 4 - 6 weeks. If the stitches irritate after two weeks, you can ask (the assistant of) your doctor to remove them. You may shower freely from the day after surgery.
Some women have symptoms after surgery such as dizziness, insomnia, fatigue, difficulty concentrating, possibly hot flashes or back pain.
Contact
If the course of recovery after surgery is different or takes longer than previously discussed, it is wise to discuss this with your family doctor or gynecologist. In case of unexpected symptoms or concerns, we advise you to contact your general practitioner or (within the first 24 hours) consult the hospital.
During office hours, you can reach the hospital via the Obstetrics & Gynecology Outpatient Clinic, telephone number (020) 566 3400, or via the G6Noord department on number (020) 5663665. Outside office hours or in case of emergency, you can call the emergency room for women (SEH-V), located at H3Zuid, via telephone (020) 5661500.

