Who is this information folder for?This folder is intended for parents who have one or more children with sickle cell disease. It is meant to help you learn to deal with your child’s disease by providing you with information about this illness. You are not expected to read everything at once. Start with the chapters that seem most applicable to you and your child’s situation at the moment. Little by little, you may want to know more and more about the disease. At the back of this folder, you will find websites that could possibly also be useful for you and your child.There is also a folder for children between the ages of 8 and 12, as well as one for teenagers with sickle cell disease.These folders do not only contain information that is useful for your child, but also information that is important for you.
Index
Chapter 1: The sickle cell team 4
The pediatric haematologists 5
The educational services of Amsterdam UMC 5
Chapter 2: The out-patient clinic 5
The first out-patient visits 5
Checking the cerebral blood vessels 7
How does the brain test actually work? 7
Chapter 4: Psychosocial care in the hospital 11
Chapter 5: General information about sickle cell disease 12
Briefly, some information about our blood 12
What is sickle cell disease? 13
What are the complaints and symptoms of sickle cell disease in babies? 15
What about my child’s future? 15
Chapter 6: Symptoms of sickle cell disease 16
Painful swelling of the hands and feet 16
Pain in the bones of the arms, legs and back 16
Decreased functioning of the spleen 17
What are the signs of an acute splenic sequestration? 17
Bedwetting and night-time urination 19
Chapter 8: Medicine for sickle cell disease 22
Vaccination against pneumococcus 23
Chapter 9: Sickle cell disease and diet 23
Advice in achieving an iron-rich diet 24
What is done to determine the cause? 25
Chapter 10: Heredity and sickle cell disease 25
In brief, something about heredity 25
The hereditariness of sickle cell disease 26
Testing for carriership of sickle cell disease 29
Do the carriers themselves suffer from sickle cell disease? 29
Testing for sickle cell disease in the unborn baby 29
Testing for sickle cell disease in the newborn baby 30
Chapter 11: Exceptional treatments 30
Hydroxyurea (= Hydrea = hydroxycarbamide) 30
Removing the iron from the blood (chelation therapy) 31
Bone marrow or stem cell transplant and sickle cell disease 32
What is a bone marrow or stem cell transplant? 32
When to do a bone marrow or stem cell transplant? 32
What can the school expect and contribute? 34
What can the school do if there are problems? 35
Exercise, sports and sickle cell disease 35
The paediatric physiotherapist 36
Courses by the psychosocial department 37
Where can you go to for further information? 39
Chapter 1: The sickle cell team
In the Emma Children’s Hospital [Emma Kinderziekenhuis], we work with a team of healthcare workers in order to be able to offer you the best care we can with all aspects of sickle cell disease. Our basic principle is to make sure that you and your child can lead lives that are as normal - and as good - as possible with this disease. The team supports you in dealing with it and helps you to function as well as possible in your daily life.
In principle, we begin the counselling with a pregnant woman who is a sickle cell carrier. The support is ongoing from the earliest years up until the moment that the young person with sickle cell disease reaches the age of 18. After the age of 18, the patient is transferred to the adult sickle cell team at Amsterdam UMC, locatie VUmc. A new patient with sickle cell disease can only be registered with us via an official referral from a physician.
Our permanent sickle cell team in the Emma Children’s Hospital consists of a number of pediatric hematologists, the sickle cell nurse(s), a social worker, a (developmental) psychologist, a pedagogic staff member and someone from the educational services (hospital school). Alongside of this, we also regularly work with other healthcare workers at Amsterdam UMC, such as laboratory technicians at the vascular center and the blood lab, a pediatric dietitian or a clinical geneticist.
The pediatric haematologists
In the Emma Children’s Hospital we have several pediatricians/paediatric hematologists who are specialized in the treatment of children with sickle cell disease. Every child with sickle cell disease comes to the out-patient clinic for a check-up at least twice a year. The surgery is on Thursday mornings in waiting room 1 at the pediatric out-patient clinic. The pediatric out-patient clinic can be found on the ground floor of the Out-patient Building. The pediatric hematologist on call can be reached every day during office hours via the central number of Amsterdam UMC: 020- 5669111.
Sickle cell nurse
The pediatric sickle cell nurse can provide - as can the doctors - information about the disease to children and their parents. She supports children and their parents in dealing with this disease and in giving the medication. She is also helpful with all sorts of practical tips and advice. She - together with the social worker - also organizes a few gatherings per year with parents during which a different subject
is handled each time. In this way, you can come into contact, in an informal setting, with other parents who also have a child with sickle cell disease.
Before consulting the doctor, you will first consult the sickle cell nurse.
You can also come to the specific nurse’s surgery in waiting room 1 of the pediatric out-patient clinic. You can make an appointment for this yourself or do this in consultation with the sickle cell nurse. The pediatric sickle cell nurse can be reached via number 020-7323901. She can also be reached via e-mail at: kindersikkelcel@amsterdamumc.nl
The educational services of Amsterdam UMC
The permanent contributor of the educational services from the sickle cell team keeps track of the school progress of the children with sickle cell disease. She lets the school know about the disease, provides the school with advice on supporting the child as well as possible and passes any questions that the school may have onto the pediatrician. She can be reached via telephone number: 020-5668952.
Social worker
We have a committed social worker who, for several days per week, counsels the children with sickle cell disease and their parents. She can be reached via the secretariat of the psychosocial department: 020-5665674.
Pedagogic staff member
From the psychosocial department, there are pedagogic staff members available to accompany your child when it must have a blood puncture in order, for example, to have blood transfusions or blood drawing. They will also support your child during admission for a painful crisis.
Chapter 2: The out-patient clinic
The first out-patient visits
Your child has recently been diagnosed with sickle cell disease. Because sickle cell disease is both a chronic and a hereditary disease, this generally evokes a variety of emotions in the parents. Because it is you who have passed on this disease, you may, perhaps, feel guilty. Perhaps grief and anger are at the forefront, emotionally. This could be, for example, because the future of your child and your family has suddenly become more uncertain. Try not to hide or censure these feelings. It is good to know that, in time, they often - as a matter of course - become less severe. You will learn to deal with them better. Ultimately, you will start to feel better again.
The important thing is how you deal with your feelings. What can you do? The first step is to make yourself aware of your feelings. Sometimes, you need help from others - such as your partner, family members or friends - to clarify your feelings. It is often a good idea for parents to share their feelings with others, for example, with other family members or friends, a fellow-sufferer or, perhaps, someone from their church. It is sometimes a good idea to get professional help from, for example, a social worker or a psychologist.
You will, of course, also be given the space and opportunity in our clinic to talk to the consulting pediatrician about your feelings. In order to feel better, many parents profit from learning more about sickle cell disease. It is possible that you are dealing with faulty ideas about the disease.
Perhaps the disease is less severe than you imagined. It often emerges that there is a great deal that you can do yourself to help your child. As you learn more about the disease, you will also be able to care for your child better. You are then also better able to allow others to care for your child.
In the beginning, you will come with your child to the out- patient clinic every two to three months for a check-up and in order to give you the opportunity to ask your questions. You will then gradually get to know the consulting pediatricians and the staff nurse. It is always possible to contact the clinic in-between visits if there are problems or if you have any questions. For babies, we take a blood test every six months. As your child gets older, the visits to the out- patient clinic will be reduced to twice a year, with blood testing once a year.
Further out-patient visits
Sickle cell disease is a chronic illness. That means that it is not curable. In order to prevent your child from landing in a sickle cell crisis, there is a certain regimen to be followed.
Even if your child is doing well, you must, nevertheless, come to the out-patient clinic every six months for a check- up. It is important that, during this appointment with the staff pediatrician, you report how your child is doing. If your child has had such symptoms as pain, shortness of breath or other complaints and you are not sure whether
or not these are related to sickle cell disease, it is good to mention them.
The pediatrician is interested to know:
- how often your child had a sickle cell crisis during the past period and what his or her precise symptoms were,
- the number of times that your child had a fever,
- whether or not antibiotics were prescribed,
- how often your child was hospitalized, and whether or not your child was given blood transfusions.

Blood tests
Once a year, we also draw blood for testing. This way, we can see how the blood levels and the production of new blood are going, if there is sufficient iron and vitamin B12 in the blood and if the folic acid and vitamin D levels are good. We also look at how the kidneys and liver are functioning.
Checking the cerebral blood vessels
When your child is 2-years old, he is then eligible for a check-up of the cerebral blood vessels. This check-up is done every six months at Amsterdam UMC vascular center and takes around twenty minutes. The vascular center is located at G1-257 of the main building of Amsterdam UMC.
Why do we do this test?
Due to the sickle cell disease, the large blood vessels which must supply the brain with blood - and, thus, oxygen - can become constricted. If there is such a constriction, your child has an increased chance of damage to the brain. The damage can be prevented; for that reason your child must be checked regularly.
How does the brain test actually work?
Using sound waves, the rate of flow in the blood vessels in your child’s head is measured. This is done with a small transmitter that is placed against your child’s temple. The transmitter is connected to a monitor on which the results of the measuring can be followed by you and your child. Your child will barely be bothered by the test at all. It is not harmful or painful. The test is called: TransCranial Doppler sonogram, or: TCD.
If the outcome of the TCD test is not good, your pediatrician will notify you. She will then tell you what the next step is going to be.

TransCranial Doppler sonogram (TCD)
X-ray examination
When your child is 15 years old, he will be given a chest X- ray to examine his heart and lungs. We will also do an ECG and a sonogram of the heart because the heart can become somewhat enlarged due to the anemia. Moreover, we will also do a sonogram of the abdomen in order to examine the abdominal organs, such as the liver, kidneys and spleen and to see if there are gallstones.
Eye examination
It is sometimes necessary to pay a visit to the ophthalmologist to have the eyes examined.
Chapter 3: Visiting the A&E department of Amsterdam UMC. If your child has such symptoms as pain or fever that have started - or increased in severity - outside of office hours, you can go to the A&E department of Amsterdam UMC . A number of things are then important:
- It is preferable to first call the pediatric junior doctor on duty (to be reached via Amsterdam UMC telephone switch board: 020-5669111);
- this can save you an unnecessarily long wait: If it is, for example, very busy the doctor can suggest that you come a bit later.
- the doctor can sometimes advise you over the phone so that you and your child do not need to come in.
- Do not forget to say that your child has sickle cell disease.
- If your child is in pain, make sure that he/she is given a painkiller before you go to the A&E department (or take extra pain medication with you to the A&E department). If you must wait for an unexpectedly long time, this ensures that your child is not without pain medication and is in pain unnecessarily.
- Make sure that you always have a sufficient supply of pain medication at home.
Hospitalization
It is sometimes necessary to admit your child to the hospital. That could be because it is no longer possible to treat the symptoms at home, but it could also be because your child needs surgery. For all information concerning the routine during hospitalization, you can read the booklet: Hospitalization in the Amsterdam Medical Centre Emma Children’s Hospital. When your hospitalization is planned, this booklet will be sent to you at home and, in the case of an emergency hospitalization, you will receive it in the ward. You will also be given extra information about the nursing ward. If you have not received it, do not hesitate to ask for it.

Admissions interview
On the ward, the nurse will ask you about any medication your child is taking (please bring this with you in the original packaging), allergies and your child’s diet, as well as how you normally deal with your child. This is, in particular, focused on any particulars that, in your opinion, are important in order care as well as possible for your child. Every child who is admitted to the hospital receives a bracelet with his or her personal details.
Sleeping rooms
In every ward, there are rooms with one, two or four beds. Depending upon the reason for admittance, your child will be put in a room by himself or with other children. A nurse will show you the ward: the rooms, the playroom or the lounge. The doctor and doctor-in-training (an intern) will talk to you about your child’s symptoms, about previous periods of illness, possible medication usage and the family background. They will then give your child a physical examination and, possibly, draw some blood.
Support
How a child reacts to hospitalization depends upon his or her nature, age, previous experiences and preparation. Together with you, we would like to try to help your child through this period as well as possible. The doctor, the nurse and the pedagogic staff member each have their own task in the daily treatment of and care for your child. It goes without saying that they will involve you in this as much as possible. You will also be given the opportunity to participate in the daily round with the doctors and nurses on the ward. Moreover, on the ward they will pay careful attention to how your child is processing the hospitalization.
It is generally known one day in advance when your child will be examined or treated so that you can adjust your schedule to that. You can consult with the doctor, nurse and pedagogic staff member about whether or not you will be present during tests and procedures. One parent may always spend the night with your child.
It is important that your child continues to develop as normally as possible during the hospitalization. For that reason, the Children’s Hospital offers a wide range of play activities and the opportunity to continue with school. Play materials and educational tools are available in all shapes and sizes. The hospital television station or Emma Children’s Television has its own TV programs that are made for and by children in the Emma Children’s Hospital.
Going home
Generally, the patients are discharged from the hospital in the mornings. Before you leave with your child, you will first have one more meeting with the doctor. During that meeting, you will be given guidelines about possible medication, diet and matters that it is best to allow or forbid. You will, if necessary, also be given additional guidelines for care from the nurse or the pedagogic staff member. If you child still needs nursing care, the nurse will discuss that with you. A so-called transfer nurse can organize the necessary care for you. And finally, you will also be given an appointment for your next visit to the out-patient clinic.
It is possible that your child will still need a bit of time to process everything that has happened in the hospital. Some children are suddenly afraid of being left alone, have problems getting to sleep or start wetting their beds again. In general, these reactions will disappear after a short time. If you have the idea that it is all taking too long, you can then contact the pedagogic staff member who supported your child in the hospital.
Chapter 4: Psychosocial care in the hospital
Psychologists and social workers at the Psychosocial Department provide help to children (and their parents) when psychosocial problems arise in relation to the disease. Moreover, help is provided to patients with specific physical symptoms for which it is known that, alongside of medical care, psychological treatment is also necessary. In order to receive help from a psychosocial department staff member, an appointment must always be made beforehand with a doctor at the Emma Kinderziekenhuis. Requests for assistance are always made by the consulting physician.
Medical social work
The medical social workers are focused on the support and counselling of the parents in adjusting to the disease and to the treatment of their child (parental support). They also collect data about the family situation, insofar as that is relevant to providing good care for the child. They also mediate and advise in the case of practical problems in relation to
the medical care of the child, for example, problems related to the parents’ work or health insurance. The social workers refer the parents, where necessary, to other care agencies.
Psychologist
If necessary, you can also receive help from one of the pediatric psychologists. They are focused on study and treatment of children who have emotional and/or behavioral problems. They also organize (on line) discussion groups and courses for patients, their parents, brothers and sisters.
Pedagogic care
Pedagogic staff members are focused on the prevention of problems in development and parenting, which arise as a consequence of the disease and treatment during the child’s hospitalization. The pedagogic staff member contributes to the daily care of the child and prepares the child and the parents for tests and procedures. She also helps the child to
process the hospital experience through play therapy, discussions and leisure activities.
Introductory visit
In order to prepare a child as well as possible for a stay in the hospital, there is the opportunity for the parents, together with the child, to come to the hospital for an introductory visit. An appointment for this can be made with the head of Pedagogic Care via the departmental secretariat. Telephone: 020-5665674.
Fear of needles
The pedagogic staff member can be consulted during hospitalization, but also at the out-patient clinic, on problems concerning the treatment, such as difficulty taking medication or a severe fear of needles or procedures. A special child-focused approach may solve this problem.
Chapter 5: General information about sickle cell disease
Who has it?
Sickle cell disease chiefly occurs among people originating from tropical and subtropical countries, such as Africa, the Mediterranean area (specifically, South-East Turkey and the Middle East), South and Central America (Caribbean area) and parts of Asia.
Because the Netherlands are becoming increasingly diverse and colorful, we are seeing a higher incidence of sickle cell disease in this country. Probably around 1500 people - mainly children and young adults - in the Netherlands are afflicted with sickle cell disease. Somewhat more than half of the people with sickle cell disease in the Netherlands originate from Ghana or other African countries, the Netherlands Antilles, Curacao, Mediterranean or Asian regions. Somewhat less than half of them originate from Suriname.

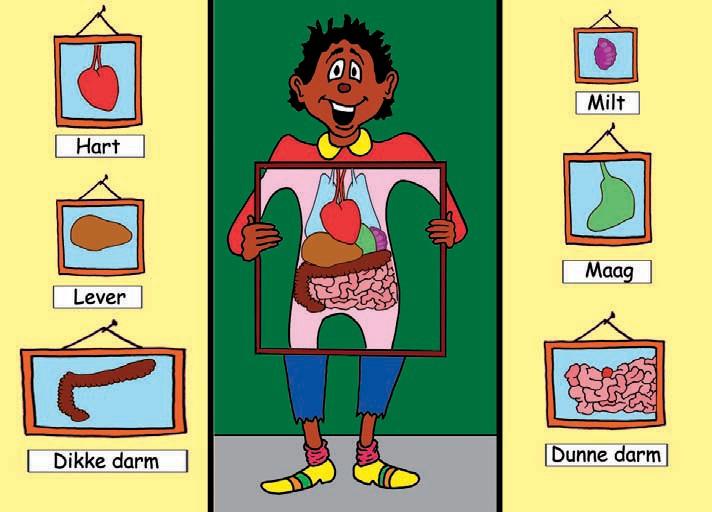
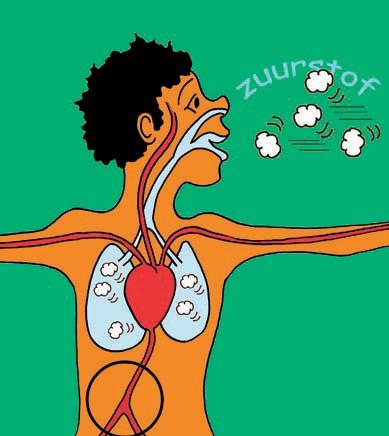
Briefly, some information about our blood
The task of our blood is to transport substances, gasses and cells throughout the body. An adult has approximately five liters of blood, of which more than half is fluid (plasma). The rest of the blood is made up of blood cells. There are red blood cells (erythrocytes), white blood cells (leukocytes) and platelets (thrombocytes). The red blood cells contain hemoglobin - the red protein - that can bind oxygen. The oxygen, bonded to the hemoglobin in the red blood cells, is transported throughout the body. The red blood cells have a limited lifespan in the bloodstream: around 120 days.

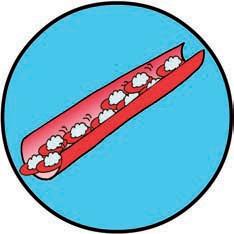
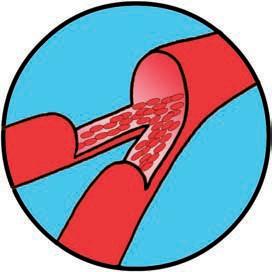
Blood vessel with red blood cells and oxygen
What is sickle cell disease?
Sickle cell disease or sickle cell anemia - is a hereditary form of chronic anemia that can lead to serious medical problems. Treatment and regular check-ups - at least twice a year - by a physician who is well-versed in sickle cell disease is, therefore, advisable. In people with sickle cell disease, the hemoglobin in the red blood cells is a bit different than in other people. A slight change in the hereditary material causes a deviating form of hemoglobin to be produced instead of the normal hemoglobin. Instead of the normal coin shape, these red blood cells can take on a half-moon or sickle shape, thus the name sickle cell (Figure 1).
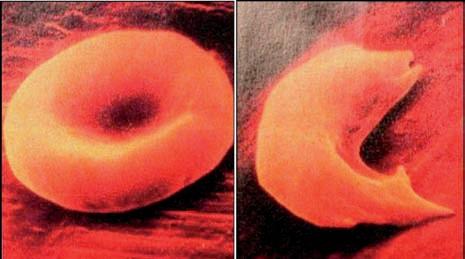
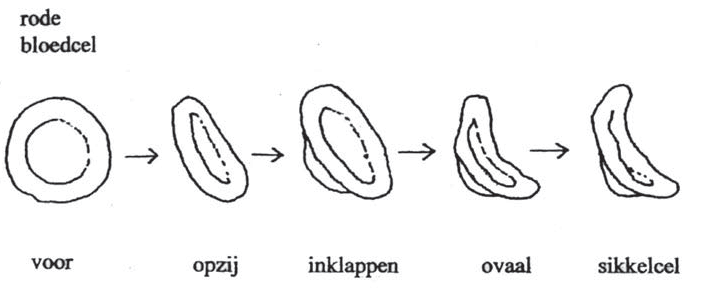
Figure 1.
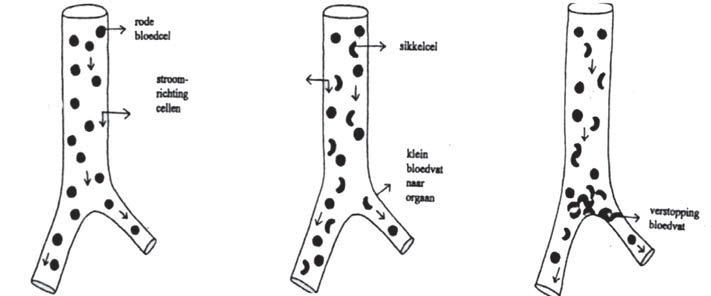
Because of this abnormal shape, the red blood cells are broken down more quickly (after 30 days) than normal (after 120 days). Because of this faster decomposition, people with sickle cell disease almost always suffer from anemia. The most important symptoms of anemia are: fatigue, listlessness, lack of energy, heart palpitations and, sometimes, ringing in the ears. A waste product of the hemoglobin protein, a yellowish coloring (bilirubin), is then released, which causes a yellowish tint to the skin and the eyes. This discoloration is called jaundice. Not only are the deviant red blood cells more quickly broken down but, due to their special sickle shape, they also have the tendency to hook together easily. This causes the development of clogging in the blood vessels (Figure 2).
someone without with sickle cell disease sickle cell disease
sickle cell disease in a calm situation in a ‘crisis’
Figure 2. The development of sickling in a blood vessel
The sickling can develop because of an increase in the need for oxygen in the body, such as with major exertion or exhaustion (for example, through gym, swimming, sports,
lack of sleep), through infections (colds or flu, for example), through shortage of oxygen (for example, by staying at high elevations), through dehydration (due to vomiting, insufficient fluids or diarrhoea) or during severe cold: if your child is not dressed warmly enough or after swimming. The symptoms that someone with sickle cell disease has are closely related to where in the body the blood vessels become clogged. Clogging can occur in the bones, the spleen, the lungs, the intestines, the brain, the kidneys, the penis and the eyes.
Clogging can cause severe pain and tissue damage (Figure 3).
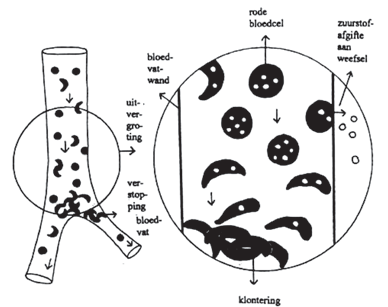
Figure 3. The sickling in a blood vessel in a ‘crisis situation’ (enlargement)
What are the complaints and symptoms of sickle cell disease in babies?
It is exceedingly important that sickle cell disease be diagnosed as early as possible in a baby in order to prevent complications. For this purpose, from January 2007 on, all children born in the Netherlands are screened for sickle cell desease. This neonatal screening takes place within a few days after birth. At birth, a baby with sickle cell disease does not yet display any symptoms of the disease. This is because, at birth, there are still a great many healthy red blood cells present that every unborn child makes himself (foetal blood cells) and still too few deviating red blood cells. During the first six months, the healthy (foetal) red blood cells in a baby with sickle cell disease are gradually replaced by sickle cells. (Figure 4). The first symptoms can occur four to six months after birth.
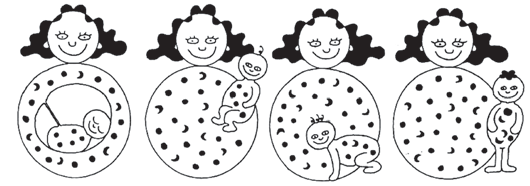
Figure 4. The course of sickle cell disease during pregnancy through to a child with sickle cell disease at the age of 1 year old
What about my child’s future?
People with sickle cell disease can lead a reasonably normal life, that means, being able to work, do sports, travel and - for women - to have children. In order to be able to lead a reasonably normal life, it is important that people with sickle cell disease receive good medical treatment and are well supported by their doctors, family and friends. Medical care with many different specialists can ensure that the complications of sickle cell disease are recognized and treated at an early stage.
Chapter 6: Symptoms of sickle cell disease
Painful swelling of the hands and feet
Approximately one third of the children with sickle cell disease younger than three years old are afflicted with painful swelling of the hands and/or feet. This is called the hand- foot syndrome. This is caused by blockage of the blood vessels in the bones of their hands and feet. We generally treat the pain at home with pain medication (suppositories) and extra fluids. The pain and swelling often pass within a few days. If your child has a fever or the pain cannot be treated at home, hospitalization may be necessary. We then administer more fluids and stronger pain medication. The hand- foot syndrome nearly always heals completely without any lingering symptoms.


Hand-foot-syndrome Normal hand
Pain in the bones of the arms, legs and back
Your child can have pain regularly as a consequence of sick- le cell disease. The pain develops because a blood vessel becomes clogged with sickle cells. The pain generally occurs in the bones of the arms, legs or back. We call this a vaso-occlusive crisis. The intestines can also become painful, which causes abdominal pain. Most of the pain caused by sickle cell disease can be treated at home. The most important remedies that are then used are:
- Drinking lots of fluids
- This prevents the sickle cells from clumping together and ensures that the clogging is dissolved. (see also the chart for fluid intake)
- Play quietly
- Have your child play quietly at home, without too much physical exertion. Bed rest is certainly not always necessary.
- Warmth
- Taking a warm bath can relieve the pain. Placing a heat pack or a warm, moist cloth on the painful place can also help.
- Massage
- Gentle massaging of an arm, leg or back can relax the child and stimulate the blood circulation.
- Pain control
- Pain medication administered according to a fixed schedule is extremely important to guarantee continuous pain relief. (see Chapter 7)
Sometimes, in spite of these measures, the pain is so severe that hospitalization is necessary. There, extra fluids will often be administered via a nose tube or an IV drip and, if necessary, stronger pain medication.
Most painful crises have no immediately damaging consequences for the arm or leg they affect. There are, however, pain crises that could be a manifestation of a more serious clinical picture and these could, indeed, have consequences for the body. In that case, immediate treatment in the hospital is necessary.
These serious crises are:
- Acute chest pain and/or shortness of breath.
- Severe abdominal pain with acute swelling of the belly (generally only occurs in children to the age of 6).
- Pain accompanied by swelling and redness in an arm, leg or back and fever (temperature above 38.5°C ).
- Sudden, severe headache.
- Pain that does not react to treatment at home.
Decreased functioning of the spleen
The spleen is an organ in the upper left side of the abdomen, just under the ribs (see picture on X-ray examination, Chapter 2). The spleen’s function is to filter out damaged blood cells and help fight infections. In children with sickle cell disease, the spleen is generally enlarged during the first years of life. In most children with sickle cell disease, the spleen decreases in size from around the age of six, due to sickling (clumping together of red blood cells) in the spleen. This causes this organ to become damaged and full of scar tissue. In some children with sickle cell disease, the spleen remains enlarged longer, sometimes even throughout their entire lives. Due to the sickling and scarring, in children with sickle cell disease the spleen does not work as well. Thus they are much more susceptible to develop severe infections with some bacterial species. This risk starts from the age of 4 months on. See also: Chapter 8.
During routine check-ups, the doctor determines the size of the spleen in order to know if the spleen is larger than normal in the case of acute illness.
In some children, the spleen swells up suddenly during an infection or fever and absorbs many red blood cells like a sponge. This can cause the blood level to suddenly drop severely. Because of the fast drop in the blood level, the blood circulation is insufficient (shock) and the child can die unless he is quickly given a blood transfusion. We call this suddenly swelling of the spleen an acute splenic sequestration.
What are the signs of an acute splenic sequestration?
Sudden, severe abdominal pain, swelling on the left side of the abdomen (distended belly), very pale color (visible at het palms of the hands and the nail-bed), extreme fatigue, dizziness, fainting, heart palpitations. If a child has had an episode of acute splenic sequestration, there is a good chance that this will happen again. Therefore, once the situation is stable, the spleen is then removed by a pediatric surgeon in an operation under a general anesthesia. It is certainly possible to live without the spleen if penicillin is taken twice a day and, in the case of a high fever, the hospital is contacted.
Anemia
People with sickle cell disease have fewer red (= containing hemoglobin) blood cells than usual. We call this anemia. Generally, a child with sickle cell disease has a hemoglobin level that is half of that of a child without sickle cell disease.
There are situations in which the number of red blood cells a child has are even lower than normal. That can happen if a child has a fever or is fighting an infection. There are two ways in which this drop in the hemoglobin level can occur:
- The red blood cells break down faster than normal (hyperhemolytic crisis); or
- The body (bone marrow) stops making new cells (aplastic crisis).
Hyperhemolytic crisis
If the blood is broken down too quickly, the child can get yellowish eyes (or the eyes become even yellower than they normally are) or yellowish skin and the urine can be darker in color (it looks like tea or cola).
When the blood level becomes too low due to the fast breakdown of the cells, it is necessary to give a blood transfusion. The following signs indicate a low blood level: Extreme fatigue, extremely pale colour (visible at het palms of the hands and the nail-bed), dizziness, fainting and heart palpitations.
Aplastic crisis
 If the bone marrow suddenly stops making new red blood cells, this is nearly always a consequence of an infection with a specific virus, the Parvo B19 virus, that also causes fever. After a few days, the infection has passed and the bone marrow starts to do its work again. If someone has had an infection with the Parvo B19 virus, he cannot get it again. When, during the infection period, the blood level becomes too low, it is necessary to give a blood transfusion. The following signs indicate a blood level that is too low: extreme fatigue, extremely pale color (visible at het palms of the hands and the nail-bed), dizziness, fainting and heart palpitations.
If the bone marrow suddenly stops making new red blood cells, this is nearly always a consequence of an infection with a specific virus, the Parvo B19 virus, that also causes fever. After a few days, the infection has passed and the bone marrow starts to do its work again. If someone has had an infection with the Parvo B19 virus, he cannot get it again. When, during the infection period, the blood level becomes too low, it is necessary to give a blood transfusion. The following signs indicate a blood level that is too low: extreme fatigue, extremely pale color (visible at het palms of the hands and the nail-bed), dizziness, fainting and heart palpitations.

Decreased growth
Some children with sickle cell disease grow somewhat less quickly than other children, right from their first year of life. This means that, during their entire youth, they are somewhat shorter and thinner than their peers. Also, the onset of puberty often comes later (sometimes even a few years later). Nearly always, these differences in height are evened out at the end of puberty. When their peers have stopped growing, adolescents with sickle cell disease continue to grow for some time. It is extremely important that your child knows that this retarded growth is part of the disease and that he will catch up later.
In order to determine if there is retarded maturation in the bones and how many years retardation this is, an X-ray of the left hand and wrist is sometimes taken. If there is a late onset of puberty, blood testing is sometimes also done to examine the level of hormones in the blood.
It is extremely important that a child with sickle cell disease eats a sufficient amount and a healthy diet. If your child is very small or thin, it may be necessary to give him extra calories. Together with a dietitian, you can decide how to do this and what kinds of extras you must offer your child. As with every child, it is important that he eats three meals a day with a few in-between meal snacks. Limit the amount of sweets as much as possible, because your child will then not have enough room for healthy food.
Bedwetting and night-time urination
We have a nice word for bedwetting: enuresis nocturne.
Why is there bedwetting?
Children with sickle cell disease are afflicted by this more often than other children. This is because the kidneys of someone with sickle cell disease have difficulty retaining fluids in the body. This develops because of repeated sickling in the kidneys. Your child does not notice this so much during the day, but at night he must urinate once or twice. Children under the age of 12 often sleep very deeply. Because of this, it is possible that they do not wake up when they need to urinate and then wet their beds. You cannot blame your child for this, but it is a troublesome problem for you, as parents, and for the child himself.
What can you do about it?
You could try to train your child - with the aid of a pad and buzzer system - to wake up from the stimulus to urinate. This is, unfortunately, not always an easy task. For children above the age of 10, there is a training program in which your child is supported daily (often by telephone) by a psychosocial staff member. Ultimately, all children with sickle cell disease are able to overcome their bedwetting. Often, they go to the toilet themselves once or twice per night.
Chapter 7: Pain control
The most important pillars in the treatment of pain with sickle cell disease is effective pain control in combination with ample fluid intake. It is important to give your child the pain medication according to a fixed schedule. Thus, there is a steady and fixed amount of the active ingredient in the pain medication in the body at all times. In this way, the pain does not keep coming back.
Below, you can find an overview of the pain medication and fluids to be administered when treating a sickle cell disease pain crisis. Everything is expressed per kilogram body weight of the child. Thus, it changes with age.
If you are in doubt about the severity of the pain, first try to manage it with the weakest pain medication. If your child continues to be in a great deal of pain, you can then try a stronger one. Fortunately, you can treat most painful crises at home. If you are not successful in treating a painful crisis at home, it may be necessary to admit your child to the hospital.
Pain control scheme
It is important to administer the pain medication at fixed times. That way, the pain killers are most effective. Thus, you do not have to wait until the pain starts again. For each of the drugs, you can choose either tablets or suppositories (whichever is most comfortable for your child). Tramadol can be administered as drops or as a tablet. The dosage and the daily frequency of administering the medication depends upon the child’s weight and is prescribed by the doctor.
For effective pain management, you can use one of the schedules below:
- For a mild painful crisis:
- Paracetamol.
- For a reasonably serious painful crisis:
- Paracetamol in combination with diclofenac or ibuprofen
- For a serious painful crisis:
- Paracetamol in combination with diclofenac or ibuprofen and tramadol (Please note: not every child will be prescribed tramadol for use at home)
Below, you will find a combination schedule for paracetamol, diclofenac or ibuprofen, in combination with tramadol if indicated:
|
For a MILD painful crisis: |
|
|
08.00 am |
Paracetamol suppository or tablet |
|
02.00 pm |
Paracetamol suppository or tablet |
|
08.00 pm |
Paracetamol suppository or tablet |
|
02.00 am |
Paracetamol suppository or tablet |
|
For a REASONABLY SERIOUS or SERIOUS painful crisis: |
|
|---|---|
|
08.00 am |
Paracetamol suppository or tablet |
|
10.00 am |
Diclofenac or ibuprofen suppository or tablet |
|
02.00 pm |
Paracetamol suppository or tablet If indicated: In combination with tramadol drops or tablet |
|
05.00 pm |
Diclofenac or ibuprofen suppository or tablet |
|
08.00 pm |
Paracetamol suppository or tablet If indicated: In combination with tramadol drops or tablet |
|
11.00 pm |
Diclofenac or ibuprofen suppository or tablet |
|
02.00 am |
Paracetamol suppository or tablet If indicated: In combination with tramadol drops or tablet |
Fluids scheme

The amount of fluids that your child must drink when treating a painful crisis:
|
Weight (kg) |
Minimal daily fluid amount (liter) |
|---|---|
|
5 |
0.5 |
|
10 |
1 |
|
13 |
1.2 |
|
15 |
1.3 |
|
17.5 |
1.5 |
|
20 |
1.6 |
|
22 |
1.7 |
|
25 |
1.9 |
|
28 |
2 |
|
31 |
2.2 |
|
34 |
2.3 |
Chapter 8: Medicine for sickle cell disease
Penicillin
In people with sickle cell disease, the hemoglobin (the red protein) in the red blood cells is a bit different than in other people. Instead of the normal coin shape, these red blood cells can take on a half-moon or sickle shape, thus the name sickle cell disease. Because of this deviant shape, the red cells hook together easily. This causes clogging in the blood vessels.
Thus, everyone with sickle cell disease develops cloggings in the spleen. This process occurs automatically and even be- gins a few months after birth. Due to this clogging, the spleen does not work as well. There is, therefore, an increased chance of serious infections with some bacteria.
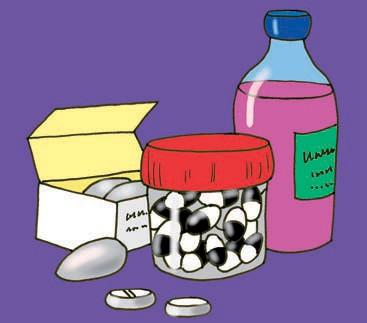
In order to strongly decrease the chance of these infections, it is extremely important that children with sickle cell disease are given extra (prophylactic) protection with penicillin. This is an antibiotic that your child must take twice a day, one dose in the mornings and one in the evenings. It can be taken in liquid or capsule form.
Ensuring that you child is consistent in taking his penicillin is one of the most important things that you can do for him. Do not stop using it because your child is doing well or, even more, because he is not doing so well. We advise you to stop giving it only on the advice of your doctor.
Folic acid
In people with sickle cell disease, the hemoglobin (the red protein) in the red blood cells is a bit different than in other people. Instead of the normal coin shape, these red blood cells can take on a half-moon or sickle shape, thus the name sickle cell disease. Because of this abnormal shape, the red blood cells are broken down more quickly (after 30 days) than normal (after 120 days). Because of this faster decomposition, people with sickle cell disease almost always suffer from anemia. The body of a person with sickle cell disease makes more blood cells per day than a person without this disease. Folic acid is a vitamin that the body needs in order to make new blood. People with sickle cell disease have, therefore, a greater need for folic acid. Folic acid is common in the foods we eat: in liver, spinach, wholegrain products and legumes. Our body, however, does not have the ability to store much folic acid. Because of this, people with sickle cell disease can develop a deficiency, which can make the anemia worse. Because of this, we advise them to take extra folic acid tablets.
Vaccination against pneumococcus
The spleen is an organ in the upper left side of the abdomen, just under the ribs. The spleen’s function is to filter out damaged blood cells and help fight infections. Because of the unnoticed sickling (clumping together of the blood cells) in the spleen, scarring occurs in this organ. Because of this, the spleen does not function as well as it should and children with sickle cell disease are more susceptible to infections. This increased sensitivity for infections starts as early as a few months after birth.
In particular, there is an increased risk of infections with the following bacteria:
- pneumococcus,
- haemophilus influenza B (HiB) and
- meningococcus.
In the Netherlands, all children are vaccinated against the last two bacteria and also against a few pneumococcal subtypes. That includes all children with sickle cell disease. Children with sickle cell disease, are also given an extra broad vaccination against several other subtypes of pneumococcus.
We call this broad pneumococcus vaccination a Pneumovax or Pneumo 23. This is generally given around the age of two and is firstly repeated after 3 years and subsequently every five years. The doctor in the hospital prescribes this vaccine and it can be administered at the out-patient clinic of the hospital or by the family doctor.
Chapter 9: Sickle cell disease and diet
A healthy, well-balanced diet provides, in principle, all the nutrients that the body needs to maintain tissue and organs and to grow, also in the case of sickle cell disease.
The table below provides a guideline with respect to the average recommended amounts of foodstuffs that are necessary to have a well-balanced diet (per age category).
|
1 to 4 years old |
4 to 12 years old |
12 to 20 years old |
|
|---|---|---|---|
|
Bread |
1-3 slices (35-105 grams) |
3-5 slices (105-175 grams) |
5-7 slices (175-245 grams) |
|
Potatoes (or rice, pasta, legumes) |
75 grams; 1.5 potatoes or serving rice/ pasta/ legumes |
100-105 grams; 2-3 potatoes or serving rice/ pasta/ legumes |
200-250 grams; 4-5 potatoes or serving rice/ pasta/ legumes |
|
Vegetables |
75 grams (1-2 spoonfuls) |
150 grams (3 spoonfuls) |
200 grams (4 spoonfuls) |
|
Fruit |
1.5 fruits (150 grams) |
2 fruits (200 grams) |
2 fruits (200 grams) |
|
Dairy products |
300 ml milk(products) and 10 grams of cheese (½ slice) |
300-450/600 ml milk (products) and 10-20 grams of cheese (½-1 slice) |
500 ml milk (products) and 20 grams of cheese (1 slice) |
|
Meat (lunchmeat) fish, chicken, egg or meat substitutes |
50 grams |
50-100 grams |
100-120 grams |
|
Low-fat margarine, margarine, bake and fry products |
15 grams |
15-35 grams |
20-30 grams |
|
Beverages |
0.8 liters |
1-1.5 liters |
1.5 liters |
There are, however, a number of things that need special attention with sickle cell disease:
Iron
Iron is one of the substances in haemoglobin. Haemoglobin absorbs oxygen in the lungs and it is then transported to all the cells in the body. An insufficient amount of iron in the blood means that the oxygen provision is not as good as it should be. Thus, it plays a role in the metabolic processes in the blood and the cells of the body. Iron is a mineral and the body gets its minerals though food. It is important to make sure that children with sickle cell disease eat iron-rich foods.
Advice in achieving an iron-rich diet
- Iron from animal products is absorbed better by the body than iron from vegetable products. Iron-rich animal products are: Meat, fish, chicken, lunchmeats, cheese, liver, liverwurst, meat paste and pâté. Vegetable products are: Bread, rice/pastas, vegetables, legumes, nuts and seeds.
- Iron from vegetable products is absorbed better by the body if it is eaten together with vitamin C-rich foods, such as citrus fruit (orange juice, grapefruit juice, lemon or kiwi) rosehip syrup, rosehip jam and sweet bell peppers.
- Try to introduce a greatly varied diet with all types of fruit, meats, fish and poultry. Iron-rich vegetables are: Endive, artichokes, broccoli, courgette, peas, purslane, turnip greens and oyster plant.
- Coffee and tea can inhibit the absorption of iron if it is drunk during mealtime. Therefore, preferably drink these beverages between meals.
- Special iron-rich products, such as rosehip syrup with added iron (for example, Roosvicee Ferro) have a function in a diet that does not contain sufficient iron. The iron in the syrup is absorbed best when it is mixed with water, fruit juice or fruit sauce/salad.
- A few examples of iron-rich snacks are: Cold cuts, piece of sausage, snack biscuits such as Evergreen or a whole wheat cracker with cold meat.
- Limit the intake of cookies, candy, chips and sodas. These products decrease the appetite and do not supply any valuable nutrients.
Folic acid
The body needs folic acid (B9) to maintain growth and for the production of red and white blood cells. For good folic acid intake, it is important to eat a varied diet with sufficient vegetables (especially green vegetables and asparagus), fruit, bread and grain products and legumes. In order to limit the loss of folic acid when cooking, it is advisable to cook foods in as little water as possible.
Vitamin B12
Vitamin B12, or cobalamin, is necessary for the production of red blood cells and for a well-functioning nervous system. Vitamin B12 is the only water-soluble vitamin that is stored in the body. Vitamin B12 can only be found in animal products (thus, in meat, fish, chicken and dairy products). A deficiency of this vitamin in the diet only becomes clear after a long time because the body first uses up the supply that it has stored itself. A shortage can ultimately lead to a form of anemia (pernicious anemia) and to tingling in the fingers, memory loss, coordination disorders and muscle weakness in the legs.
What is pica?
Your child has pica if, over a long period of time, he eats things that are not meant to be eaten. That could be various things, such as dirt, paper, foam rubber, sponges, chalk, paint or other things.
What causes pica?
Around one third of the children with sickle cell disease suffer from pica. The precise cause is not known. Pica is more common among children with a lower hemoglobin level and among children who are underweight. It is sometimes caused by undernourishment or an iron or zinc deficiency. Often, however, this does not appear to be the case. Your child can also suffer from serious pica because things are not going well at home or at school or because he feels very depressed. Sometimes there is someone in the family who has also suffered from pica. If your child has pica, this can cause stomach pains, damage to the teeth or poisoning.
What is done to determine the cause?
We measure the iron and zinc levels in the blood. If these are both normal and your child still has serious pica symptoms, there are possibly psychological reasons for it.
What do we do to help your child recover from this?
If we do not know exactly why your child suffers from serious pica, someone will go to talk to him/her and to you, as parents. We want to know if there are things that are bothering your child or things he is not happy about. We believe that your child has somehow learned the pica and, therefore, can also unlearn it. The child psychologist can help you and your child with this.
Chapter 10: Heredity and sickle cell disease
In brief, something about heredity
Every person is made up of cells and every cell contains 23 pairs of chromosomes, that means, a total of 46 chromosomes. These chromosomes contain the hereditary material (genes). At conception, half of the chromosomes of the father are coupled to half of the chromosomes of the mother and, in this way, passed onto the child. At conception, the ovum of the mother contains 23 chromosomes and the sperm cell of the father also contains 23 chromosomes. In the fertilized ovum, the hereditary characteristics (genes) are, therefore, doubly present: from the father and from the mother.
The hereditariness of sickle cell disease
Sickle cell disease appears mainly among people who originate or whose ancestors originate from tropical and subtropical countries and also among people from countries around the Mediterranean Sea. The presence of this disease in (sub)tropical countries is connected to the fact that the gene that causes sickle cell disease provides, at the same time, a partial, ‘natural’ protection against malaria. Someone who inherits the gene for sickle cell disease from one parent is called a carrier. A carrier himself has no problem with or symptoms of sickle cell disease.
Carriership of a hereditary disease is nothing unusual. Every person is a carrier of one or more hereditary diseases without noticing or knowing anything about it. Someone does not actually get sickle cell disease unless he or she inherits the sickle cell gene from both parents. Sickle cell disease is an example of an illness that, in medical terminology, is an ‘autosomal recessive’ disorder. ‘Autosomal’ means that the disease can occur in both boys and girls. ‘Recessive’ means that the disease can only be inherited if both parents are carriers of the gene that causes the disorder. In order to demonstrate all the possibilities of inheritance, the following drawings each portray four children.
In Figure 1, the symbols are given that are used to explain the carriership of sickle cell disease.
Figure 1. The symbols that explain the hereditary characteristics.
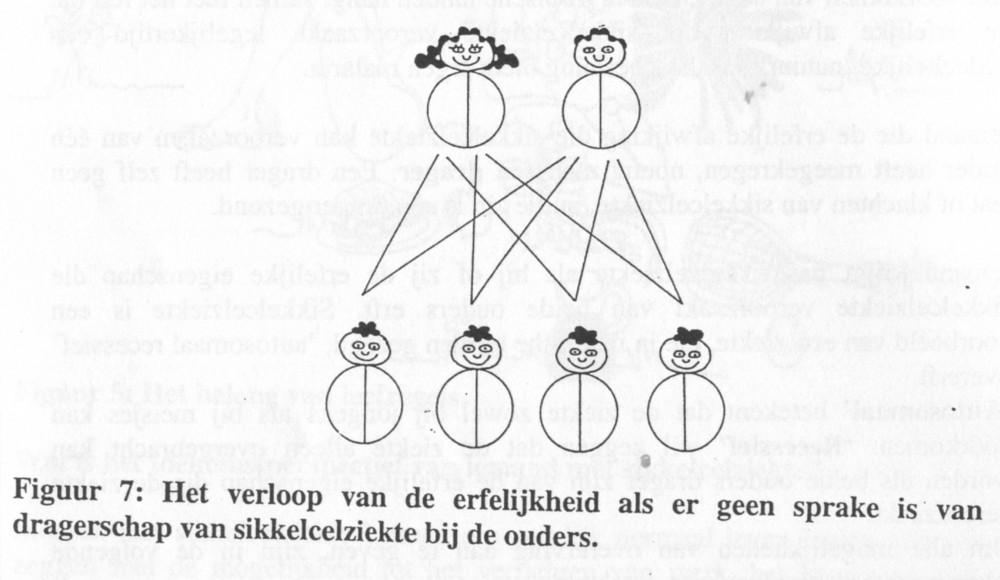
Figure 2: The course of heredity if there is no question of sickle cell disease carriership in the parents.
Figure 2 shows how the heredity takes place if there is no question of sickle cell disease carriership in the parents. The children of these parents receive half of their genetic characteristics from the mother and the other half of their genetic characteristics from the father. If neither parent is a carrier of sickle cell disease, no child of theirs will, therefore, be born with sickle cell disease or be a carrier.
Carriership of sickle cell disease can occur in either the man or the woman. A carrier of sickle cell disease has, himself, no problems with the disease and no symptoms; in that sense, a carrier is healthy. If only one parent (father or mother) is a carrier, then each child will have a 50% chance of also being a carrier. If only one parent is a carrier, a child cannot, however, get sickle cell disease, itself.
In Figure 3, we see that both parents are carriers of the gene that causes sickle cell disease. For each pregnancy, there is a 25% chance - or 1 in 4 - that a child will be born that is neither a carrier of sickle cell disease nor has the disease itself. There is a 50% chance - or 1 in 2 - that a child will be born who is a carrier of sickle cell disease. Finally, there is a 25% chance - again, 1 in 4 - that a child will be born who has sickle cell disease himself. This child has inherited the gene that causes sickle cell disease from both the father and the mother, so he carries the gene twice.
These chances return with each pregnancy. It is possible that if a first child is born with sickle cell disease, the next child will also have it. But it is also possible that, in the next four pregnancies, children are all born without sickle cell disease. A child with sickle cell disease is born healthy, that is, without symptoms. The first symptoms can occur four to six months after birth.
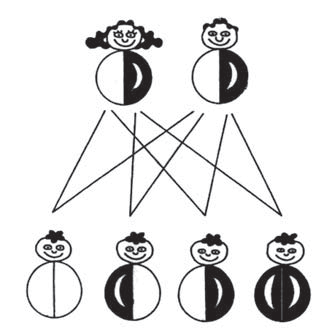
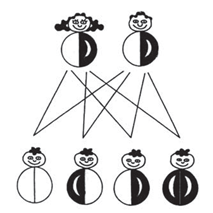
Figure 3. The course of heredity if both parents are carriers of sickle cell disease.
It is also possible that one of the parents has sickle cell disease (in figure 4, which is the woman) and the man is a carrier of the sickle cell disease. In this situation, the chance of a child with sickle cell disease at each pregnancy is 50% - 1 in 2. The chance of having a child who is a carrier of sickle cell disease is then also 50% - 1 in 2.
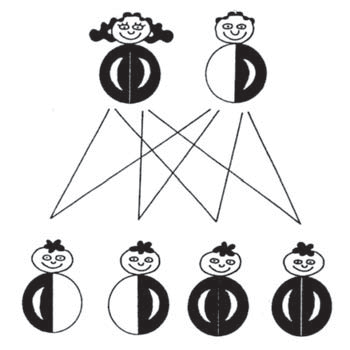
Figure 4. The course of the heredity if the woman has sickle cell disease and the man is a carrier
In Figure 5, the man has sickle cell disease and the woman is not a carrier. In this situation, there is no chance of a child with sickle cell disease, but all of the children are carriers.
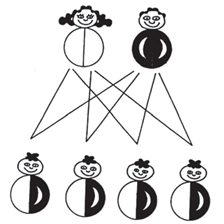
Figure 5. The course of the heredity if the man has sickle cell disease and the woman is not a carrier.
Testing for carriership of sickle cell disease
When someone originates from a country where sickle cell disease is common or knows that sickle cell disease (or sickle cell carriership) occurs in the family, it is advisable to have a blood test done to test for carriership of the disorder. This test can be done at any age and is requested by the various doctors involved (such as family doctors, the pediatrician, the hematologist) or by the midwife.
If both parents are carriers of sickle cell disease, they can be referred for genetic counseling to one of the specialized departments at one of the academic hospitals, the so-called Clinical Genetics Centers. Via these centers, prenatal testing can also be done, if desired. Your specialist, generally a pediatric hematologist or gynecologist, can tell you what the possibilities are and provide you with a referral.
Do the carriers themselves suffer from sickle cell disease?
It has already been stated above that carriers themselves do not have sickle cell disease. Carriers are healthy. Only very extreme situations, such as the running of a marathon at high elevation, flying in planes with no pressure cabin or parachuting can cause problems among carriers.
Testing for sickle cell disease in the unborn baby
Parents who are both carriers of the gene for sickle cell disease run the risk of having a child with sickle cell disease. For that reason, it is possible to test the foetus for sickle cell disease early in pregnancy. The most common way to test for this is by means of chorionic villus sampling. For chorionic villus sampling, the parents must, in the seventh week of pregnancy - or as soon as possible after that - be referred to a Clinical Genetics Centre.
In chorionic villus sampling, done around the twelfth week of pregnancy, a small amount of tissue (chorionic villus) is removed from the placenta. This tissue, just like the baby, originates from the fertilized ovum and has, therefore, the same genetic characteristics.
With this tissue, DNA testing is done (testing of the genetic characteristics) in order to see if the as yet unborn child will develop sickle cell disease. When doing this, it is also necessary to draw blood from the parents in order to do DNA testing on them and to compare this with the DNA of the baby. The results of this DNA test will be available approximately two weeks after the chorionic villus sampling. If, from the chorionic villus sampling, it emerges that the as yet unborn child will indeed develop sickle cell disease, the parents can decide to have the pregnancy terminated. This is then done around the fourteenth week of the pregnancy. In the case that a pregnancy termination is seen as undesirable and the parents have decided beforehand not to do this, then, in most cases, no chorionic villus sampling will be done. There is, namely, around 0.5% chance of a miscarriage from the chorionic villus sampling itself.
Testing for sickle cell disease in the newborn baby
If no test has been done prenatally to see if the child will develop sickle cell disease, this can be done at the time of delivery or shortly afterwards. Since January 2007, all children born in the Netherlands are tested for the presence of sickle cell disease. This is done my means of the heel prick test that your child is given between the third and seventh day after birth. In this way, if the child has sickle cell disease, the doctor can begin treatment on time and, in this way, in order to prevent serious symptoms.
Chapter 11: Exceptional treatments
Hydroxyurea (= Hydrea = hydroxycarbamide)
Some children with sickle cell disease have painful crises very often due to clogging of the blood vessels. At advanced age this can lead to organ damage. To prevent longterm damage and crises, already from baby age on, the pediatrician can propose a treatment with a drug that was originally used in the treatment of blood disorders other than sickle cell disease. This drug (hydroxyurea or hydroxycarbamide) is generally well tolerated and is taken once a day in the form of a tablet or capsule or a capsule dissolved in warm tea. The action is based on two effects. The first effect is that hydroxyurea stimulates the production of foetal (non-sickling) hemoglobin by the body, so that the level of sickle cells decreases. The second effect is the decrease of the clumping of the red blood cells to each other and to the wall of the blood vessels, so that the chance of clogging (crises) decreases.
At present we know that hydroxyurea is a safe treatment even for babies from 9 months on and that this treatment can prevent complications of the disease at a later age.
If your child is being treated with this drug, during the starting phase we check his or her blood several times per year for the foetal haemoglobin (HbF) levels and any possible side-effects.
Red blood cells in the blood vessel
Blood transfusions
Children with sickle cell disease sometimes need extra blood. If we give someone blood, we call this a blood transfusion. It is sometimes even necessary to give your child a blood transfusion every month. We call this a chronic blood transfusion scheme.
Various problems come to mind that make it necessary for your child to be treated with a chronic blood transfusion scheme. This is, for example, the case if it has been determined that your child has a stenosis in one or more of the cerebral blood vessels. Also, such a chronic transfusion scheme is started if your child has had a cerebral infarction. Now and then it happens that a child is started on a chronic transfusion scheme if he or she is having a great many serious and painful crises in quick succession.
Your child then comes to the out-patient treatment clinic every month in order to receive a blood transfusion for a number of hours, and then goes home or back to school. Moreover, your child’s blood is also monitored regularly.

Removing the iron from the blood (chelation therapy)
Children with sickle cell disease sometimes need extra blood. If we give someone blood, we call this a blood transfusion. Various problems come to mind that make it necessary for your child to have a blood transfusion. It is sometimes even necessary to give your child a blood transfusion every month. We call this a chronic blood transfusion scheme.
If this is continued for more than about a year, there is the chance that too much iron is stored in the body. This extra iron can cause damage, most importantly to the heart and liver. It is then necessary to take special chelation medication.
At present we have effective tablets available, which your child has to swallow or chew on a daily basis. The name of this product is called deferasirox.
Sometimes these tablets are insufficient or your child can’t maintain the daily intake of them. In that case a (complementary) treatment with Desferal (= deferoxamine) can be indicated.
The worst part of the treatment with Desferal to remove the iron from the body, is that it must be administered via an SC pump (generally during the night) under the skin and takes 8-10 hours to complete. It is generally given 5 days per week (sometimes seven days per week). The treatment can be given at home and is looked after by the staff of a home care team. Once the treatment is well established, the decision can be made to teach you and/or your partner (and, ultimately, perhaps, your child himself) to insert the subcutaneous needle and connect the drip yourself. While the drip is going, your child simply sleeps through. The subcutaneous treatment with Desferal can, if necessary, be combined with tablets.
Bone marrow or stem cell transplant and sickle cell disease
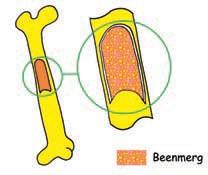
What is a bone marrow or stem cell transplant?
Blood is made in the bone marrow. This bone marrow is found inside the bones. It is here where the red and white blood cells and the platelets are made from a so-called stem cell. The young cells can develop into a red or white blood cell, or into a platelet. They then go further, into the blood. In a bone marrow transplant, the stem cells are replaced by stem cells from someone else (the donor). In order to do this, the child’s own stem cells must first be cleared out. That makes the treatment quite taxing. The new stem cells will then develop into new bone marrow that will again produce red and white blood cells and platelets. After the transplant, all of the blood cells then produced will, in principle, originate from the new stem cells.
Why have a bone marrow or stem cell transplant?
In sickle cell disease, the red blood cells take on a sickle shape under certain circumstances. Because of that, the small blood vessels sometimes become clogged and all kinds of symptoms develop, such as, for example, pain. That sickle shape develops because of an error in the stem cells. In the case of white blood cells and blood platelets,
that error does not matter, at all. It is only the red blood cells that are deviant. If the stem cells are replaced by stem cells from someone who does not have that problem, healthy red blood cells will be produced after the transplant.
When to do a bone marrow or stem cell transplant?
It all sounds so simple: replacing the stem cells of the blood. Why not do this with everyone who has sickle cell disease? That is because you cannot simply choose any donor to supply new stem cells. Everyone has a personal ‘pin code’ attached to his cells. The ‘pin code’ of the donor must, preferably, resemble the ‘pin code’ of the receiver as much as possible. If there is a great difference in the ‘pin code’, all sorts of unpleasant complications can occur.
The treatment that a child must go through in order to clear out his own stem cells also has side effects that can make a child extremely ill. Sometimes the child becomes so ill that it is necessary to admit him to the Intensive Care Unit. Every now and then, the patients become so ill that they even die but, fortunately, that is very rare. In short, you do have to pay a price for the new stem cells. Not all patients with sickle cell disease are equally ill from their condition. This means, therefore, that a balance must be sought between the severity of the disease and the severity of the treatment. And that is not necessarily the same for every patient. That is why, together with your consulting physician and the doctor from the transplant team, a decision must be made as to whether a bone marrow transplant is the most suitable treatment for your child.
You can always - via your doctor - make an appointment with the transplant specialist in Leiden to see, together, if your child is a candidate for a transplant. There is no harm in asking.
Chapter 12: Travelling

Many parents want to show off their baby or toddler to family abroad. That often means that you will be taking a plane. In general, there is no objection to this, but it is certainly important that you tell your doctor well before you go on a trip. The following matters are important here:
- A visit to the Out-patient Clinic for Tropical Diseases [Tropenkliniek] at Amsterdam UMC (020- 5663800) or to the Municipal Health Service [Gemeentelijke Gezondheidsdienst or GGD] in your place of residence. There, they know if and what extra vaccinations or medication are necessary during or preceding your stay in the tropics (Suriname, Africa, the Antilles, etc.).
- Make sure that there is a hospital within 50 km of your vacation address.
- Your own pediatrician will give you a dosage of antibiotics to take with you for emergencies; don’t forget to remind him!
- Take a sufficient supply of penicillin (Broxil) with you for daily use. Please note: Ask the pharmacist not to make up the solution for you, that way it is less perishable. You can make the solution yourself for every dosage.
- Do not forget to take a sufficient supply of folic acid and pain medication with you, in case your child has a painful crisis.
- During the plane trip, it is important that your child drinks a great deal (in any case, 10% more than normal).
- In warm countries, there is a greater chance that your child will become dehydrated. Make sure that you give him extra fluids! This is even more important if your child is vomiting and/or has diarrhoea.
- If your child is very ill, dehydrated, pale, yellowish or in pain, pay a visit to the local hospital and let them know that your child has sickle cell disease.
Of course, we wish you a good trip and a very fine vacation!
Child care
Perhaps, you are wondering if your child with sickle cell disease can go to a child care center. There is certainly no objection to this and it is up to you to weigh the pros and cons (if necessary, in consultation with your consulting physician). Contact with other children is extremely important for the development of every child. Like all parents, you wonder what the teachers will do if your child becomes ill. Here are a number of useful things to discuss with them:
- Ask the teachers to treat your child with sickle cell disease no differently than the other children.
- Discuss and explain what the signs of pain and infection are in your child. Arrange that the teacher then contacts you immediately. Make sure that you, or another trusted and informed person, are then available for consultation.
- Explain that your child must drink (and also urinate) more than other children so that attention is paid to this. Sometimes, your child needs more rest.
- It is perhaps a good idea to give the staff members an information folder on sickle cell disease so that they can learn more about the condition. This can remove a great deal of uncertainty for you and for them and provide a bond of trust. Go to the Emma Children’s Hospital, at the Emma Infotheek, for information. Information on sickle cell disease can also be found and downloaded via ‘patient folders’ at the website of Amsterdam UMC (www.amsterdamumc.nl under ‘informatie voor patiënten’ [information for patients]).
At school
What can the school expect and contribute?
Children with sickle cell disease generally do attend primary or secondary schools. It is important that the school, the teacher or the mentor, and the school doctor or nurse have all been made aware of the symptoms that can occur. Moreover, the school must be told that sickle cell disease is not contagious.
It is also important that the school adheres to the regimen that prevents symptoms, such as:
- Eating well and drinking enough at school or drinking extra fluids after extra exertion;
- Preventing over-exertion during P.E;
- Preventing the child from becoming chilled, such as ma- king sure the child is dressed warmly in the winter when playing outside or after swimming.
The problems that accompany sickle cell disease differ per child or young person. In the school-age period and during puberty, there are pain symptoms in the bones or abdomen, as well as chronic fatigue. A crisis is a situation during which the symptoms become severe and acute. If this occurs frequently, it can hinder the child’s (or young person’s) school development. Problems can occur in the areas of attention and concentration, memory, fatigue, school achievements physical condition, absenteeism, social acceptance, etc. The school should identify the problems early.
What can the school do if there are problems?
For information and advice, the school can bring in the consultant for the educational support of students with diseases. These people can be found at the academic hospital or at the educational/vocational advisory service (www.ziezon.nl ).

In the first instance, the school can start by setting up an individual plan of action. In this plan of action (opp). In this plan, the school takes into account the limitations for the student that accompanies sickle cell disease and adjusts the school programme accordingly.
For secondary school students, there are also possibilities in practical training and in the training pathway for supportive education, especially in the vmbo schools.
In the case of more serious school problems, the school can consider applying for a care arrangement for your child,. This ‘ student-bound financing can make it possible for the school to organize extra support for your child and the school can be advised and supported in this by an ambulatory counsellor. It is sometimes possible or necessary that your child transfers to a school for special education.
Students with motor skills handicaps are, if necessary, eligible for a Mytyl school (for physically handicapped children) or a Tyltyl school (if the child is also mentally handicapped). Since several years, most schools for chronically ill children have been unified with these schools.
The procedure for referral to special education is known to the internal companion/care coordinator of the school. For this procedure medical reports from the hospital can be asked for. Finally, the cooperation decides if a declaration for admittance (TLV) for special education will be granted.
Exercise, sports and sickle cell disease
Children with sickle cell disease may, just as their peers, play outside and take part in P.E. and sports! However, a child with sickle cell can endure sports less long. Playing and sports are good for the development of your growing child. Exercise is important, for improving physical condition, muscle training and limberness, as well as for the development of social skills (making friends, having fun playing together, learning to win/lose).
In order to prevent symptoms, it is important that your child:
- eats and drinks well before doing sports,
- drinks extra fluids after extra exertion,
- is allowed to indicate himself when he has had enough,
- avoids becoming chilled after playing sports (dress warmly, especially in the winter).

The paediatric physiotherapist
Because of the sickle cell disease, exercise and sports can be less self-evident. In consultation with your consulting physician, your child can be referred to a pediatric physiotherapist. This is a specialist in the area of motor functioning and movement in children and young people between 0 and 16 years old.
A plan can be set up which allows your child to continue to exercise, play and do sports, if adjusted when necessary. Your child can, for example, take individual exercise with a pediatric physiotherapist. The physical therapist can advise P.E. teachers and other instructors at school or can provide advice about various possibilities for sports and play in the neighborhood. Some examples of this include toddler gym, ‘fit kids’ (www.fitkids.nl ) and sports clubs for children with special needs. Information can be found via your municipality (for example: www.amsterdam.nl/kunst-cultuur-sport/sport ).

Courses by the psychosocial department
At the Psychosocial Department of the Emma Children’s Hospital, courses are given for children and young people with chronic diseases and for brothers and sisters of the children who are ill. The course program in the hospital is called Op Koers [‘On Course’] and via the internet Op Koers Online [‘On Course Online’] .
The purpose of this program is to teach children and young people to deal with these problems and to find solutions for them. In the courses, attention is paid, for example, to finding the correct information about the disease, learning to relax, contact with peers, dealing with worry and concentrating on their positive sides.
A course is given in groups of no more than 8 participants and is run by two psychologists. For children and young people - as well as for brothers and sisters - who are growing up with a chronic disease, there are age-appropriate groups. The course lasts 8 weeks existing of 1 meeting per week (1.5 hours per meeting).
These are the courses in the Op Koers program:
Op Pad [Getting Started] for children from 8-10-years old (primary school groups 5 and 6)
Op Stap [On the Way] for children from 10-12-years old (primary school groups 7 and 8)
Brussen for brothers and sisters from 8-12 years old (primary school groups 5 till 8)
The program Op Koers Online is a chatcourse for young people with a chronic disease, for their parents and brothers and sisters. The aim of the program is identical: learn to cope with difficult situations in relation to the disease and to find solutions for these together. This course is exclusively online and participation can be done from home.
The course is offered in groups of 5 participants in one group and is accompanied by two psychologists. The course lasts for 8 weeks (for young people) or 6 weeks (for parents and brothers/sisters) existing of 1 meeting per week (1.5 hours per meeting).
Young people Ages 12 – 18 years
Parents of children Ages 0 – 18 years
Brussen Ages 12 – 18 years
You can sign up for the courses via your pediatrician.
More information is provided at the website www.opkoersonline.nl or you can send an email to: opkoers@amsterdamumc.nl .
Did you know?
- Hemoglobin S (HbS) does not say anything about your blood type. The blood type is determined by characteristics that are found on the wall of the red blood cell. The hemoglobin is inside the red blood cells. Someone with blood type A (but also blood type B or O) can, certainly have HbS and, therefore, sickle cell disease.
- If someone has sickle cell disease and resembles his or her mother, that does not mean that he got the disease from her, alone. The gene that causes sickle cell disease is passed on from both the father and the mother.
- During a job interview, no questions may be asked about illnesses and medical history.
- A person with sickle cell disease is not eligible to be an organ donor. Sickle cell disease causes the small blood vessels to become clogged - also in the organs. Therefore, the organs are less suitable for transplant.
- There is no objection to a tattoo or a piercing on some- one with sickle cell disease (at least if you, the parents, allow it and it is done safely).
- Having the sickle cell trait means the same thing as being a carrier for sickle cell disease.
- Someone with sickle cell disease may have an alcoholic drink now and then, but never large quantities.
- Sickle cell disease is not contagious.
- People with sickle cell disease can also become parents themselves.
- It is nice if your best friend knows that your child has sickle cell disease.
- The severity of sickle cell disease has nothing to do with the gender of your child.
- It cannot be predicted if a person who had a great many symptoms as a child will have many or few symptoms later in life.
- Some people with sickle cell disease often (or always) have yellowish eyes.
- Yellowish eyes are caused by bilirubin; this is a yellow coloring that collects in the eyes and remains when red blood cells are broken down quickly and often.
- You can also be tested for sickle cell disease carriership even if you are not insured. Your family doctor can request the test in Amsterdam UMC. In Amsterdam UMC, you must first be given a patient number, and that is done via the Admittance Office [Patiëntenregistratie]. The test costs approximately 45 euro, which you must pay immediately.
Where can you go to for further information?
Patient Organization
OSCAR Nederland is a multi-ethnic foundation for carriers of sickle cell disease and thalassemia.
Oscar Nederland
Postbus 91
4000 AB Tiel
Mondays until Thursdays from 10 am– 2 pm: tel. 030-6569634
Website: www.oscarnederland.nl
E-mail: via the website
Erfocentrum
This is an information center where you can go for questions on heredity and health. The Erfocentrum is an initiative of the VSOP.
Telephone: 033-3032110
Websites: www.sikkelcel-en-thalassemie-expertise.net ; www.erfelijkheid.nl ; www.zwangerwijzer.nl
E-mail: info@erfocentrum.nl
Other sites
www.pns.nl/neonatale-screeningen/hielprik
Emma Infotheek
The Emma Infotheek is the information center of the Emma Children's Hospital Amsterdam UMC
for parents and children. You can go here for oral and written information (leaflets, books and magazines) about disease, treatment and research. If your child wants to give a speech at school about sickle cell disease or about the hospital, the employees will help your child with information.
The Emma Infotheek is located at the outpatient clinic (room A0-346). You can visit there
after you have been to the doctor and nurse with your child.
Telephone number: 020-5667959
Email: emmainfotheek@amsterdamumc.nl
The information in this booklet is also available via the website:
Kinderhematologie Patiënteninformatie Amsterdam UMC
Part of the information in this folder is derived from the brochure: Sickle cell disease: symptoms and treatment, heredity, prevention and pregnancy. Brochure for people who want to know more about sickle cell disease or sickle cell anemia. Oscar Nederland; May 2003
Final editing: Dr. H. Heijboer Illustrations (color): Dolph Paulsen


